Photodynamic Therapy with Aminolevulinic Acid Enhances the Cellular Activity of Cells Cultured on Porcine Acellular Dermal Matrix Membranes Used in Periodontology
/in Pubblicazioni recenti /da q82rrfo3Photodynamic Therapy with Aminolevulinic Acid Enhances the Cellular Activity of Cells Cultured on Porcine Acellular Dermal Matrix Membranes Used in Periodontology
Incremento della proliferazione degli osteoblasti su Lamina con Aladent
/in Pubblicazioni recenti /da q82rrfo3Terapia parodontale: casi in aumento nei prossimi anni
/in Pubblicazioni recenti /da q82rrfo3In base ad uno studio americano effettuato dalla Transparency Market Research, il mercato delle cure odontoiatriche è destinato a raddoppiare, toccando i 12 miliardi di dollari in USA. Un trend, questo, che interessa anche l’Italia, dove i casi di malattia paradontale sono in aumento.
Nell’articolo offerto da Odontoiatria33, troviamo il parere in merito del presidente SIdP Nicola Marco Sforza, che sottolinea la necessità delle campagne di prevenzione per evitare che la malattia si aggravi, nonché l’importanza della riduzione dell’invasività delle terapie, grazie alle nuove tecnologie e risorse attualmente disponibili.
Aladent contribuisce alla prevenzione e alla cura delle parodontoti. Inoltre risponde al requisito posto del presidente Nicola Marco Sforza di riduzione dell’invasività delle terapie.
Leggi l’articolo su Odontoiatria33.it
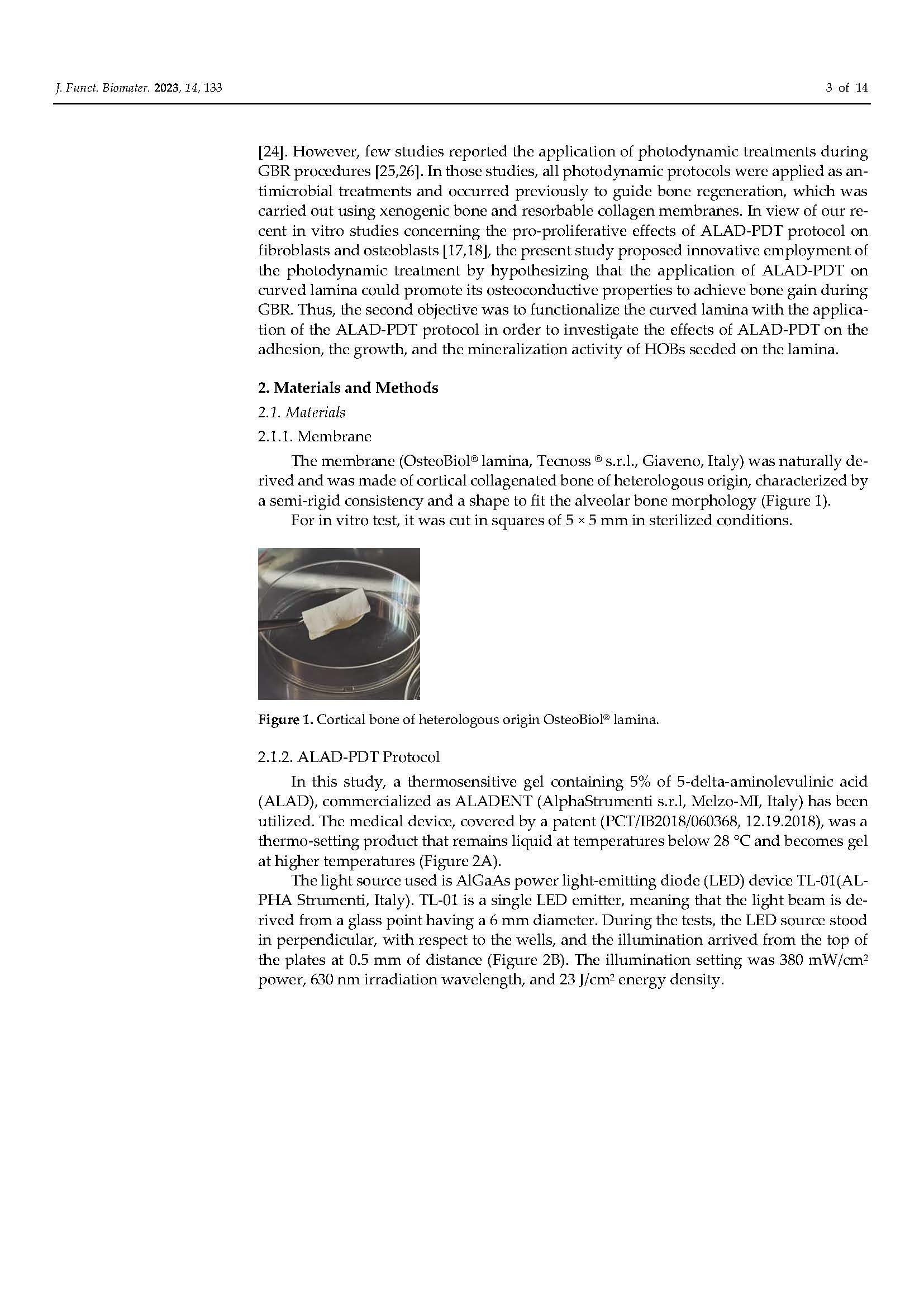
Functionalization of a Cortical Membrane with a Photodynamic Protocol
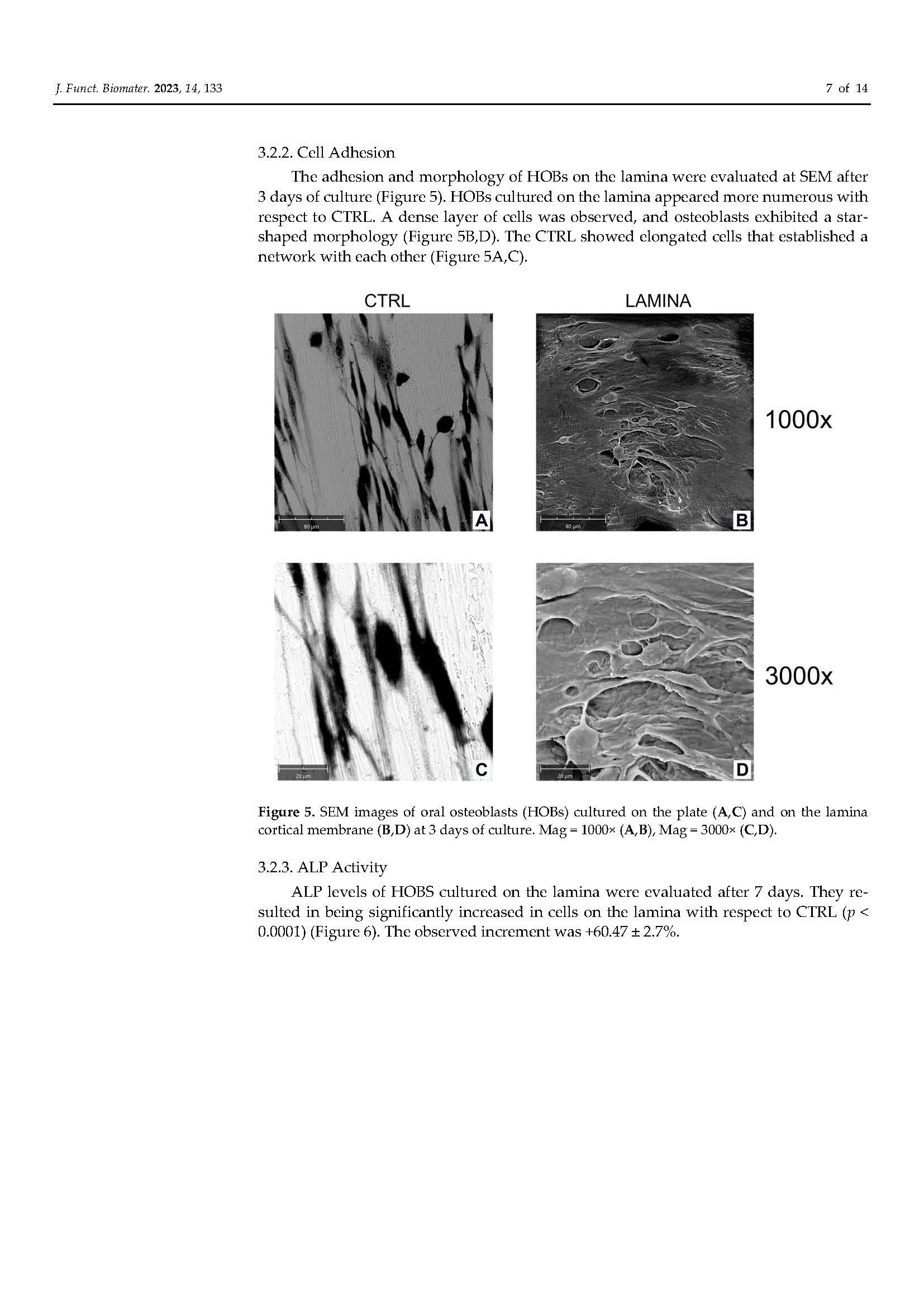
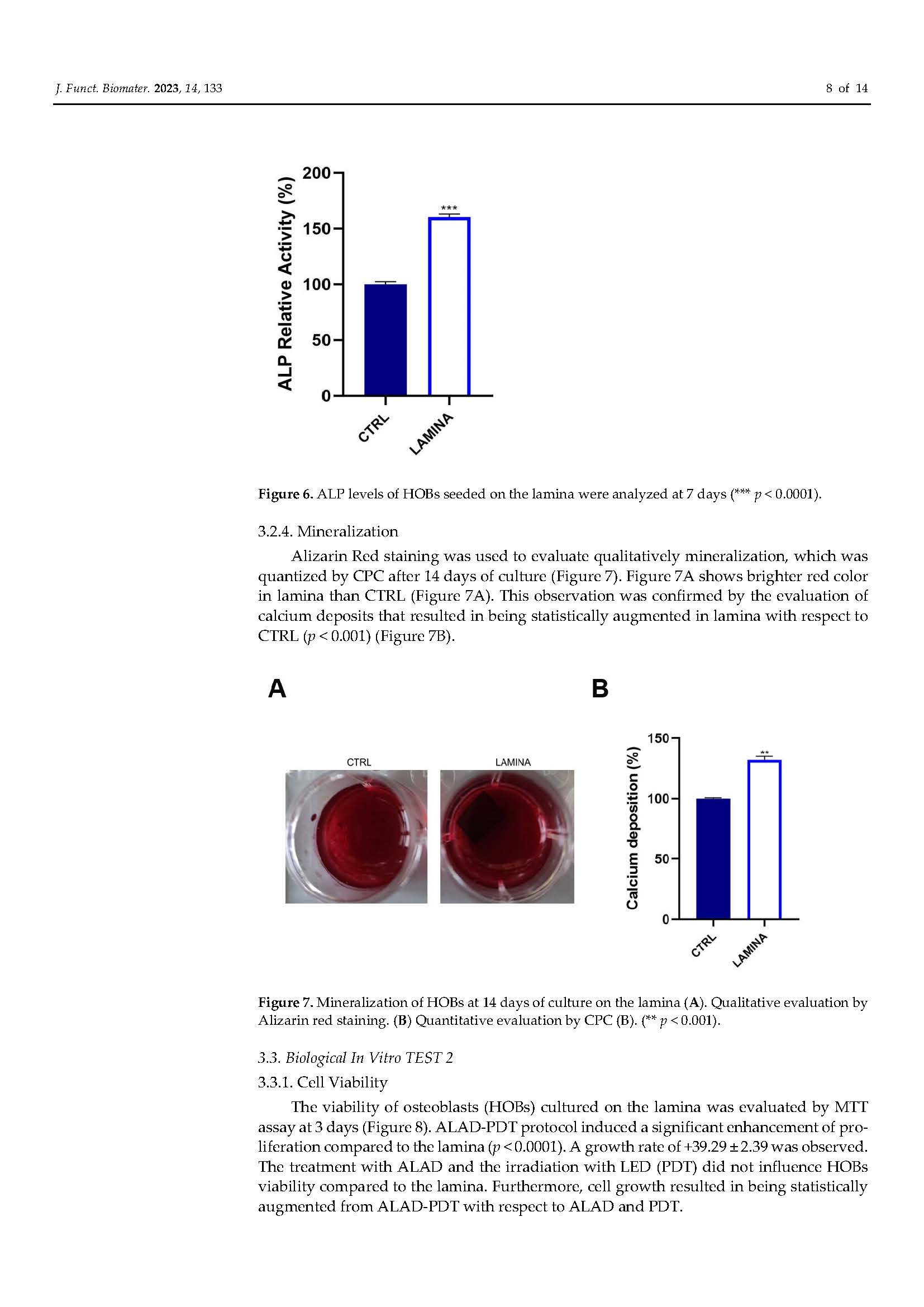
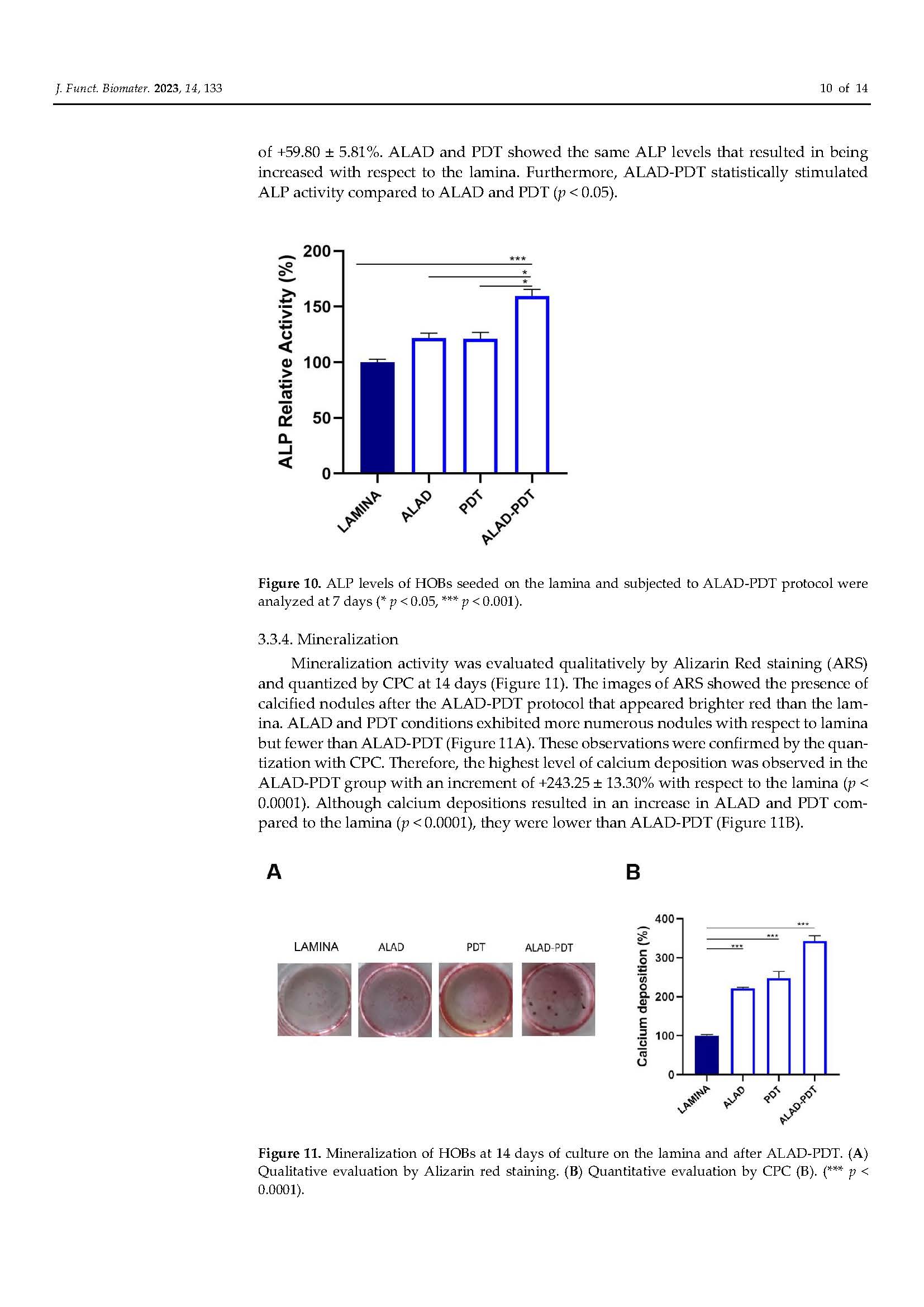
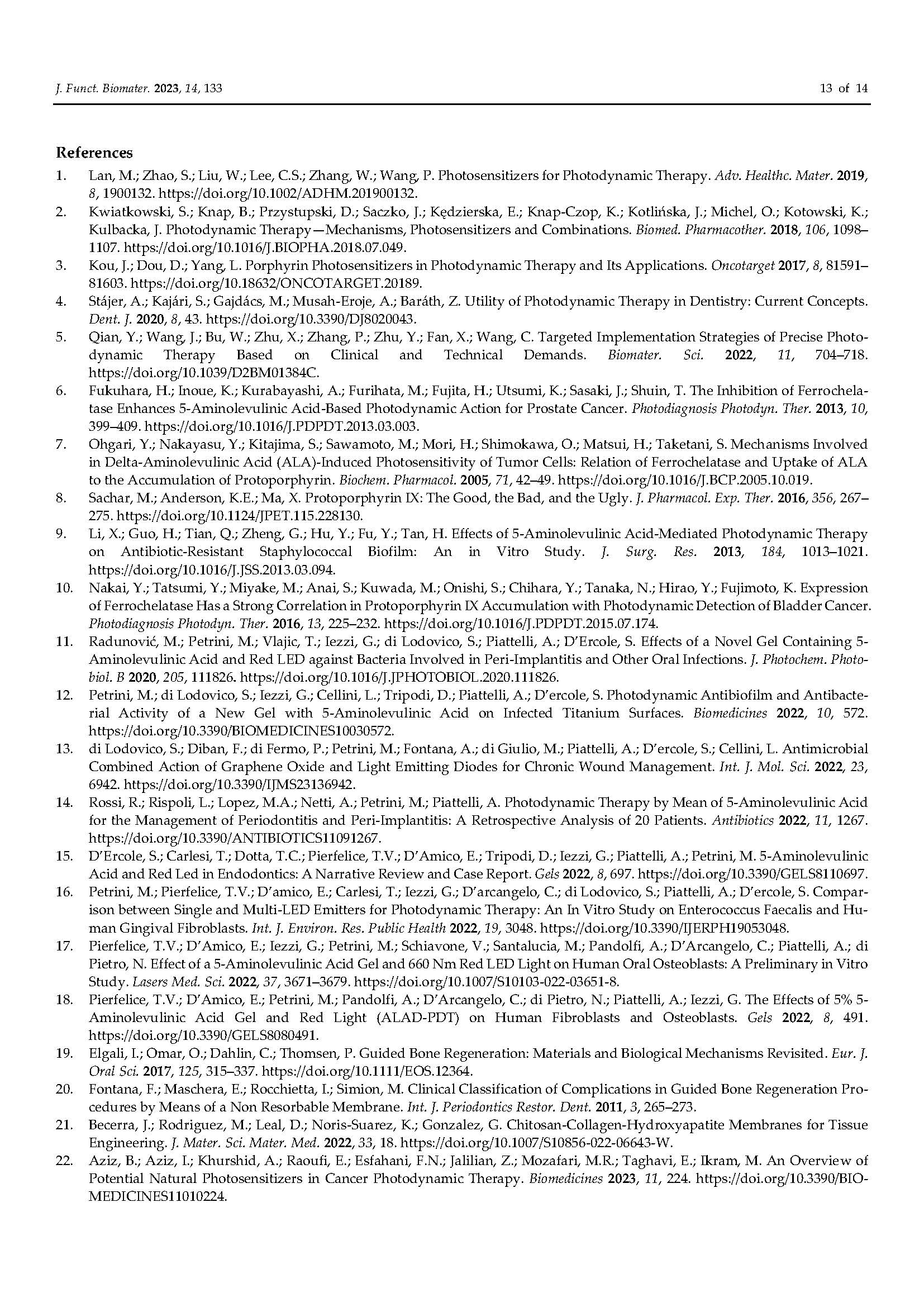
/in Pubblicazioni recenti /da q82rrfo3BONE RIGENERATION. The published article demonstrates that the adjunctive application of ALADENT -PDT to oral osteoblasts cultured on a cortical lamina provides an higher cellular proliferation and adhesion and increased matrix bone deposition. The level of calcium deposition was observed in the ALADENT-PDT group with an increment of +243.25 ± 13.30% versus the lamina alone.
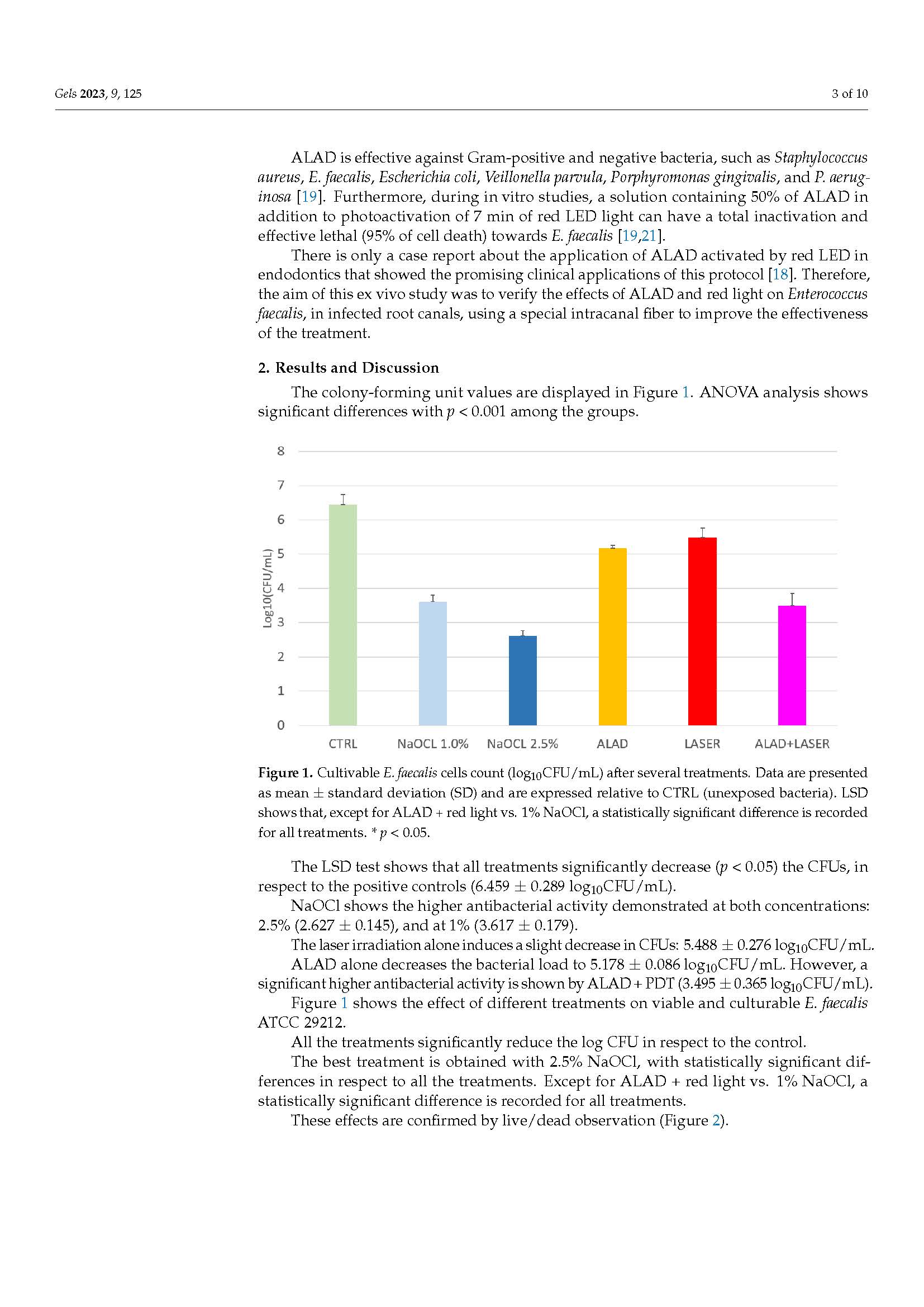
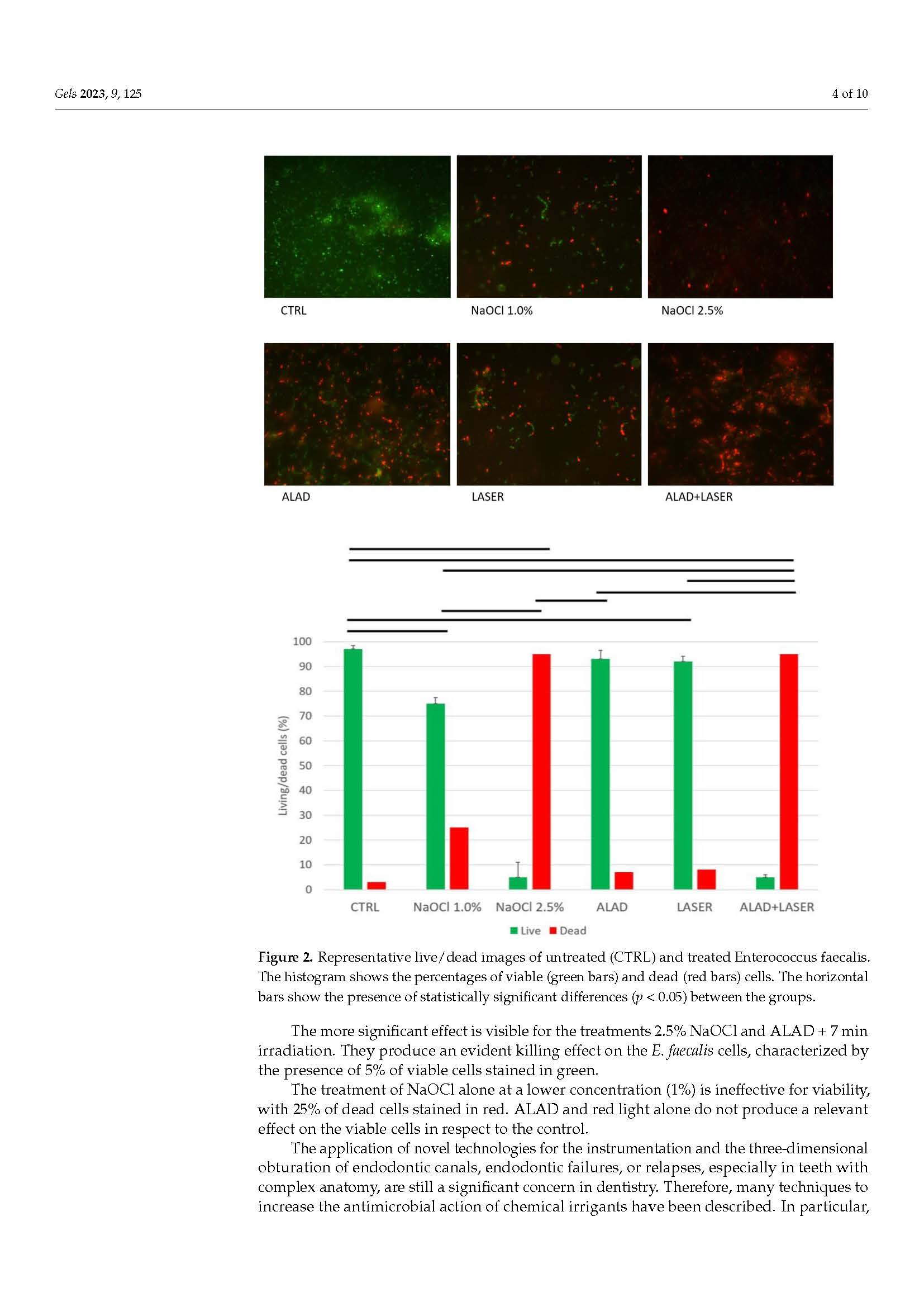
Efficacy of 5% Aminolaevulinic Acid and Red Light on Enterococcus faecalis in Infected Root Canals
/in Pubblicazioni recenti /da q82rrfo3Lasers in Medical Scienze. Original article.
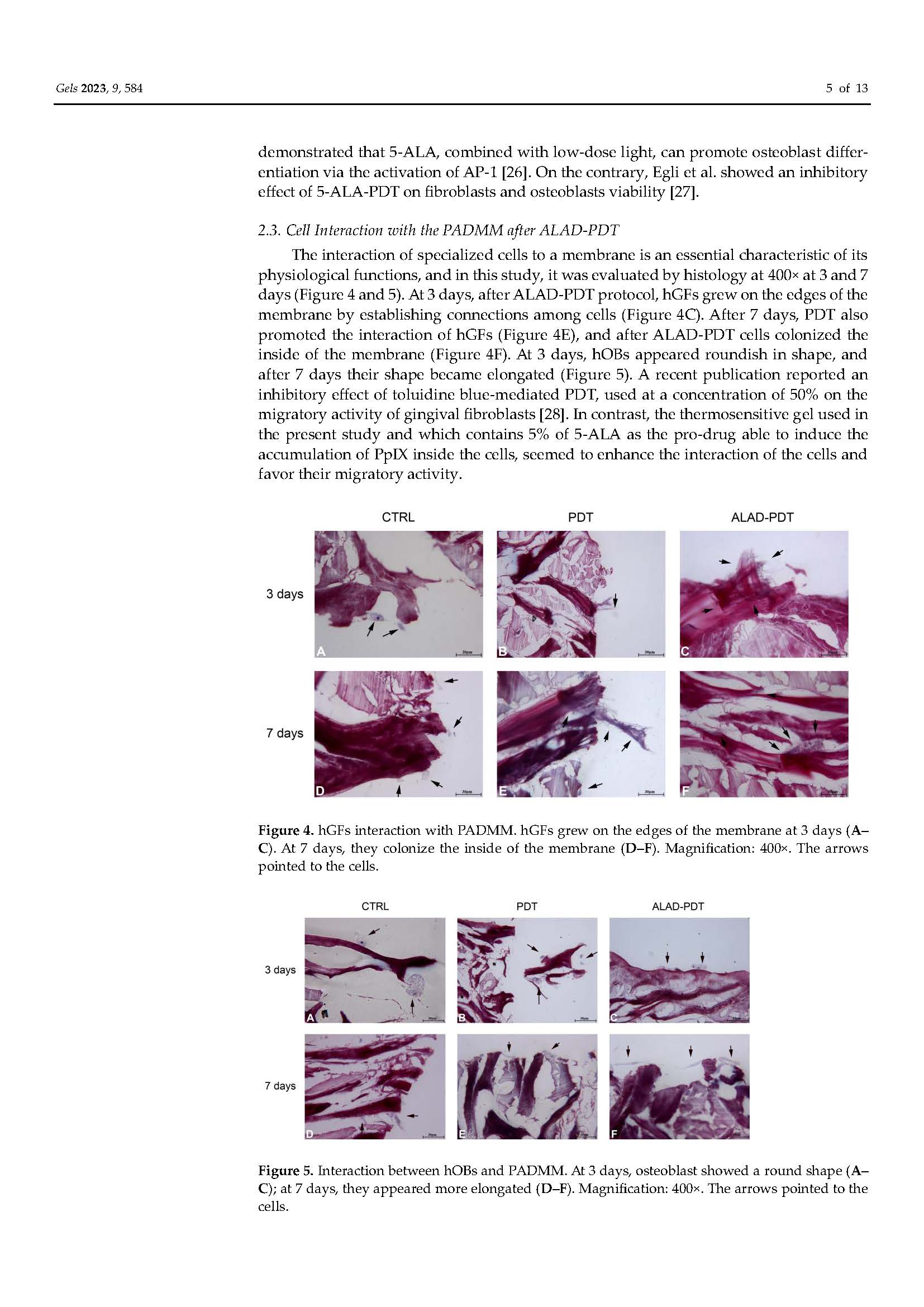
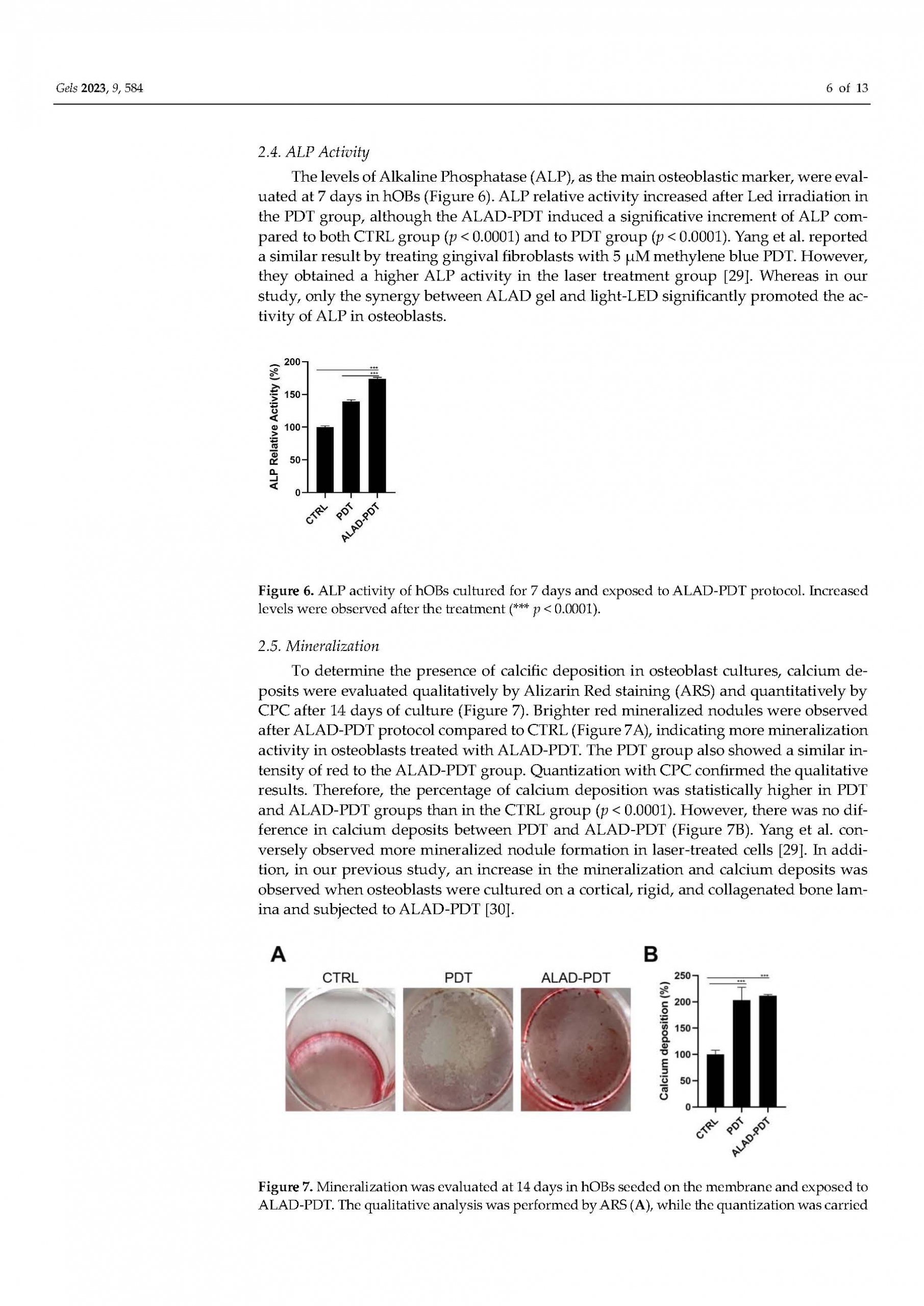
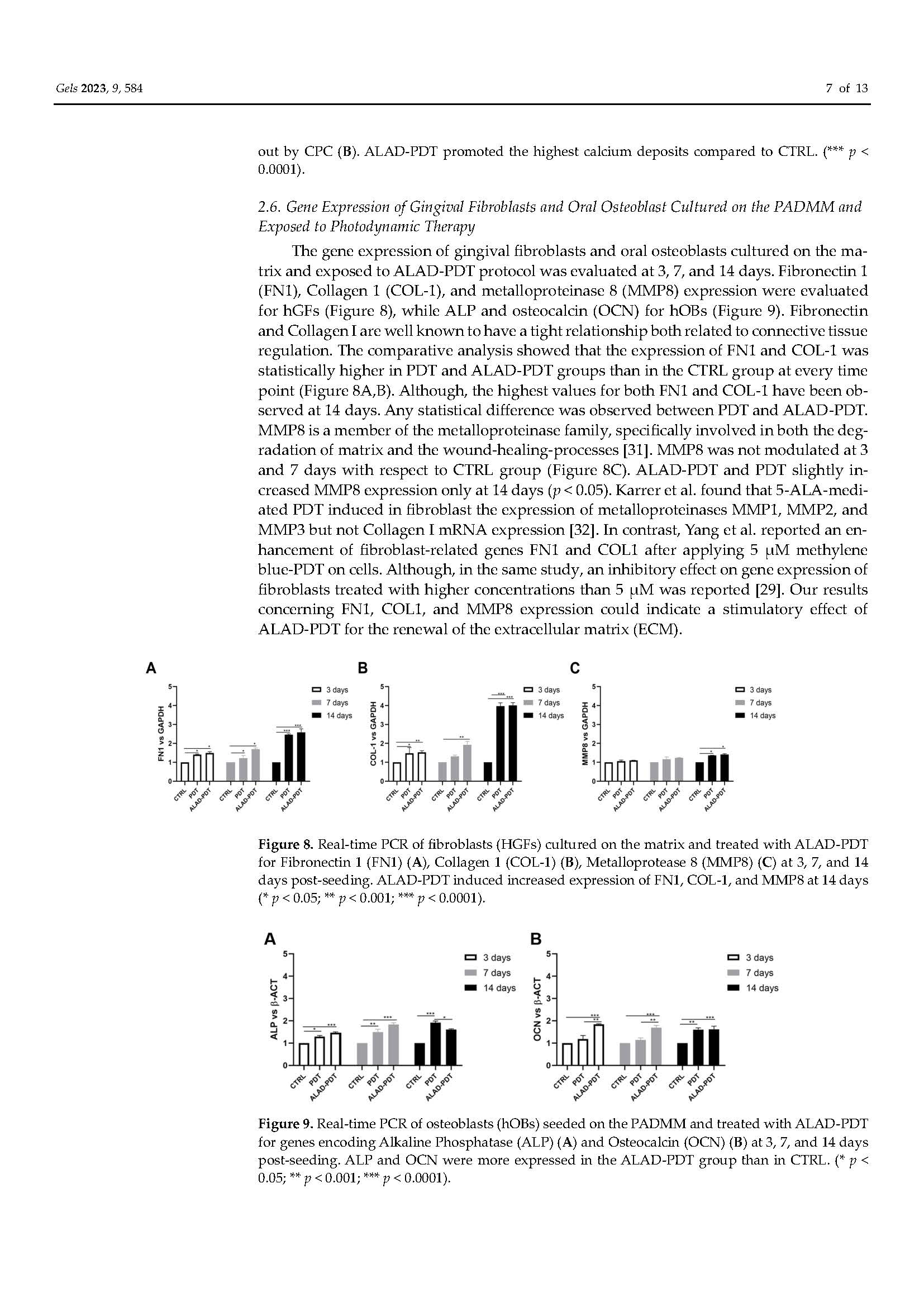
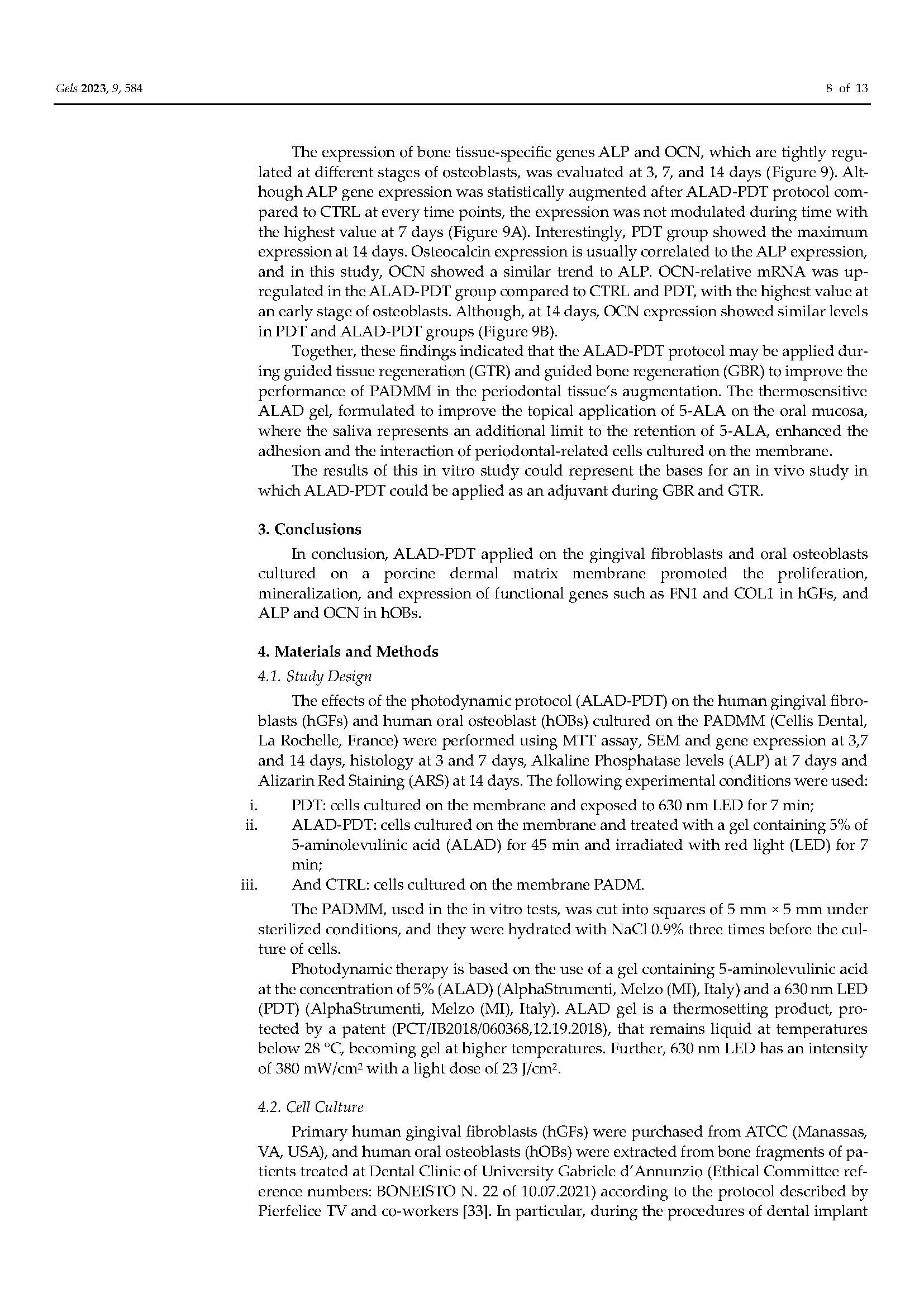
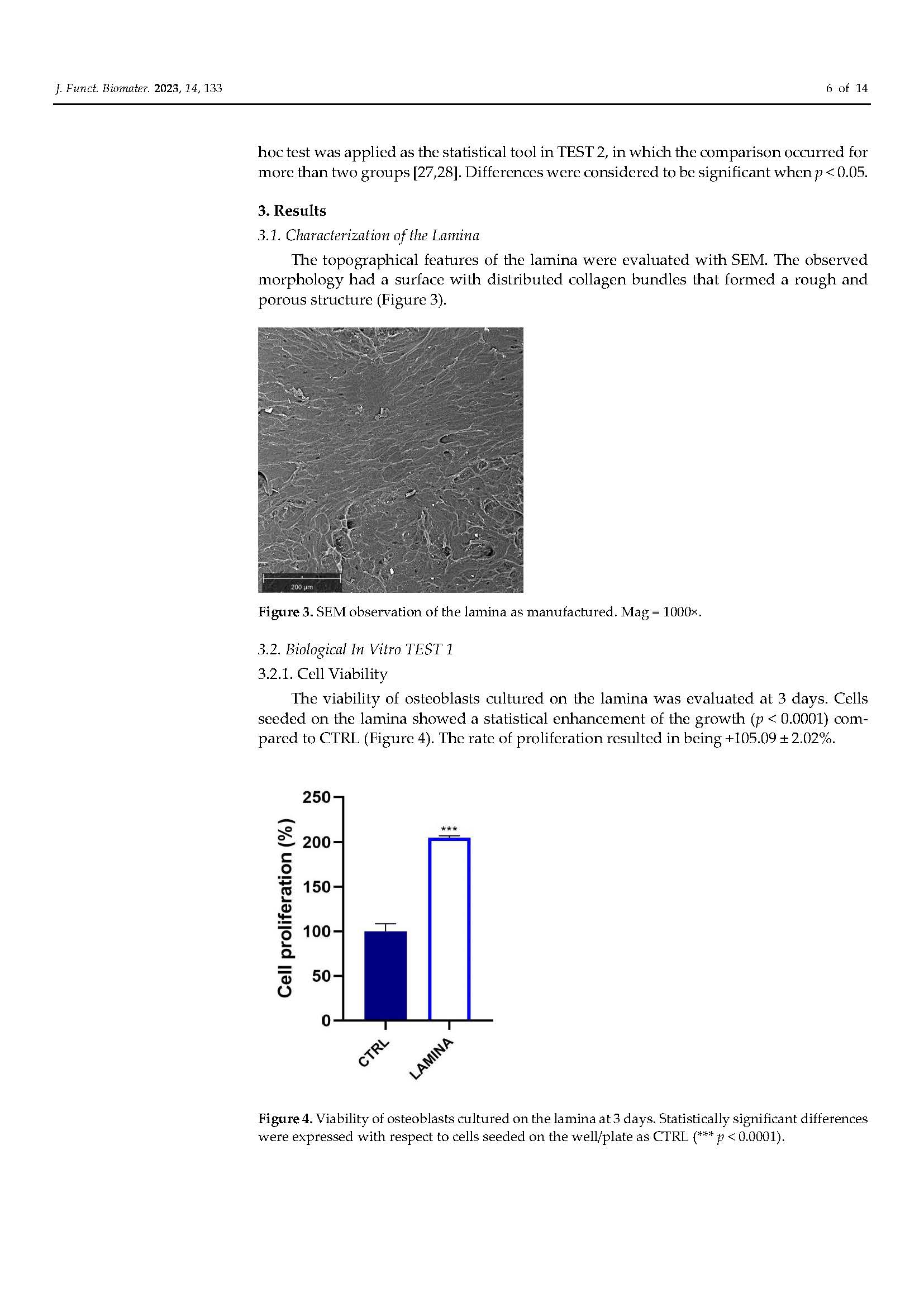
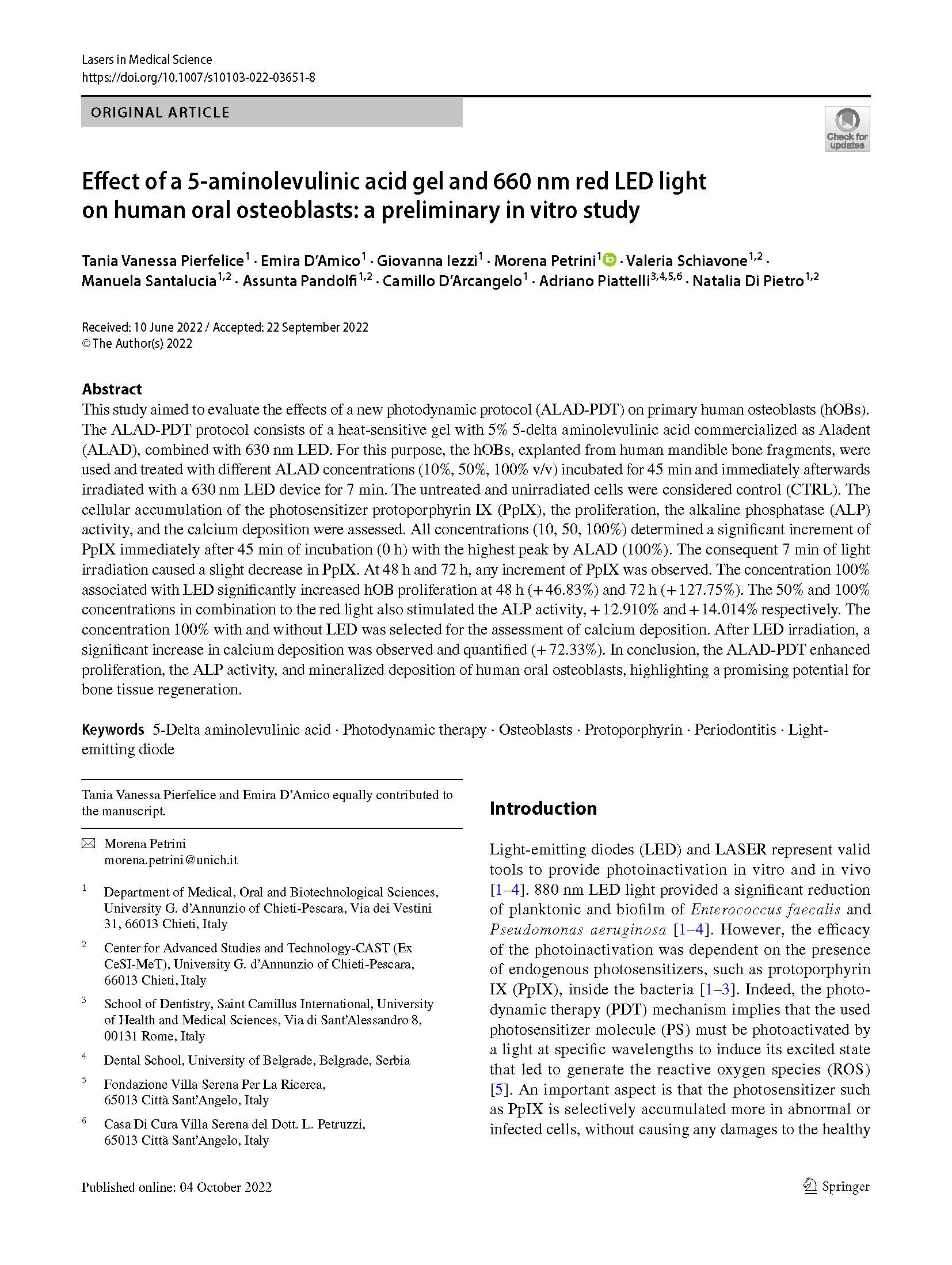
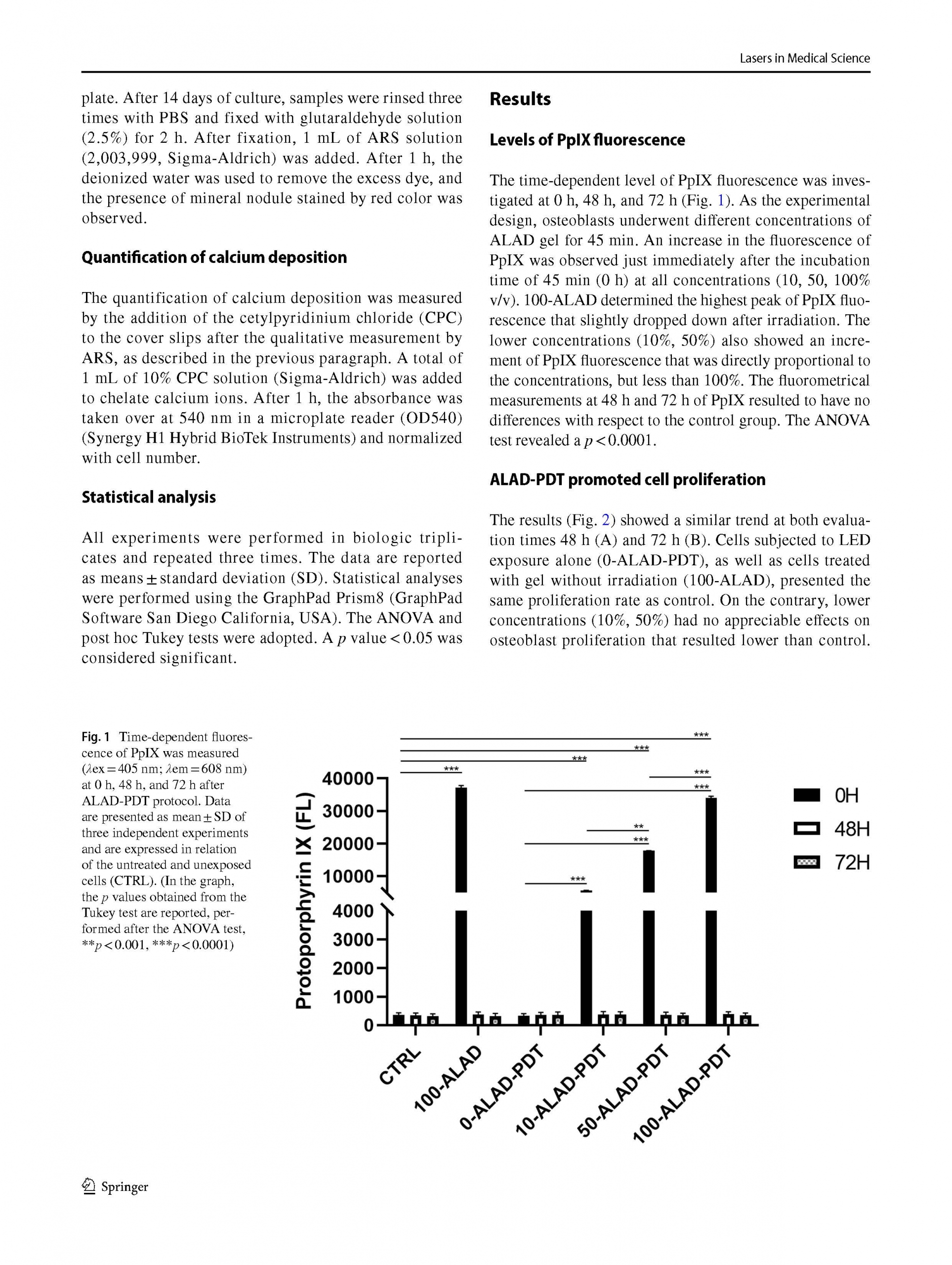
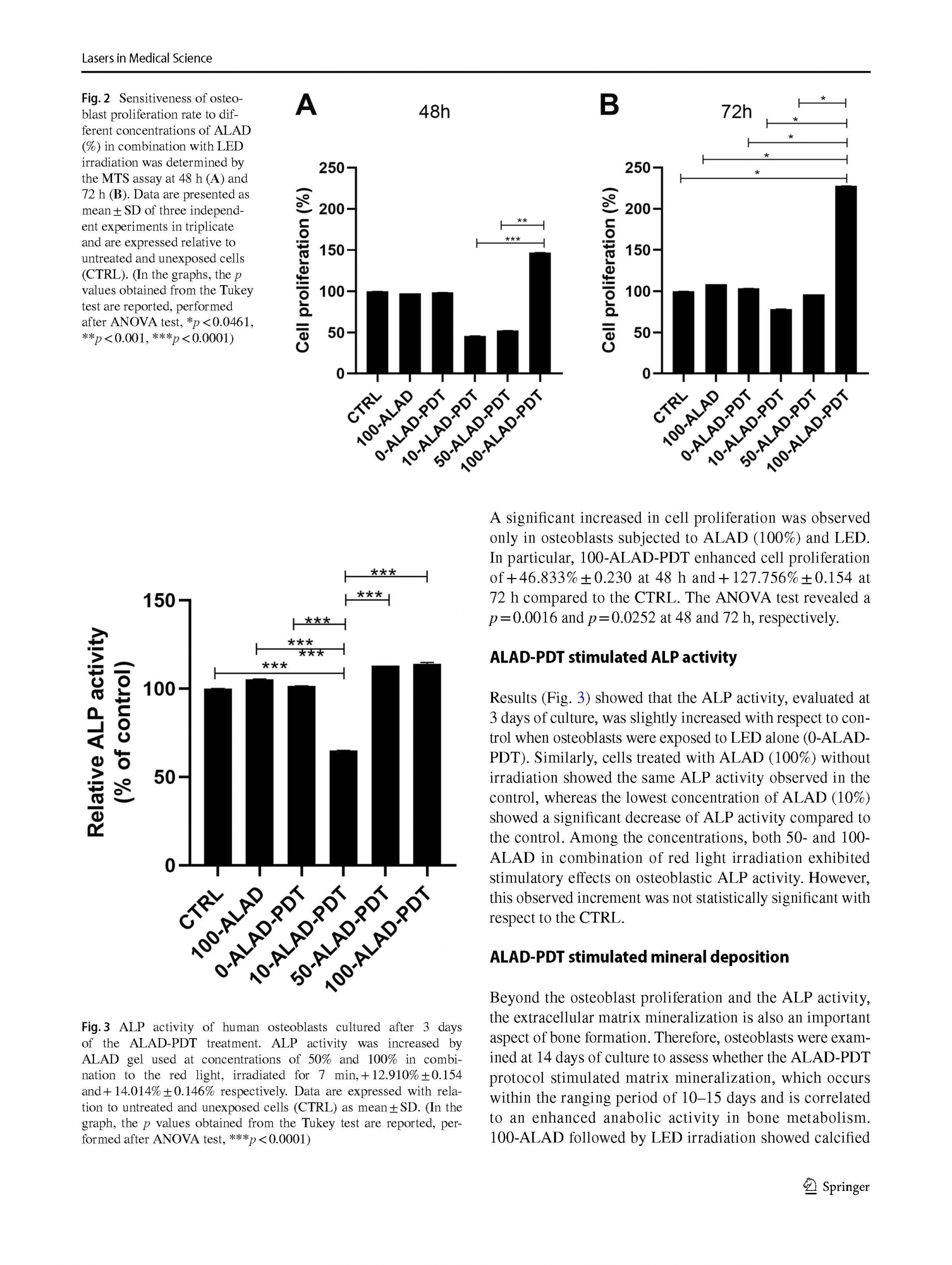
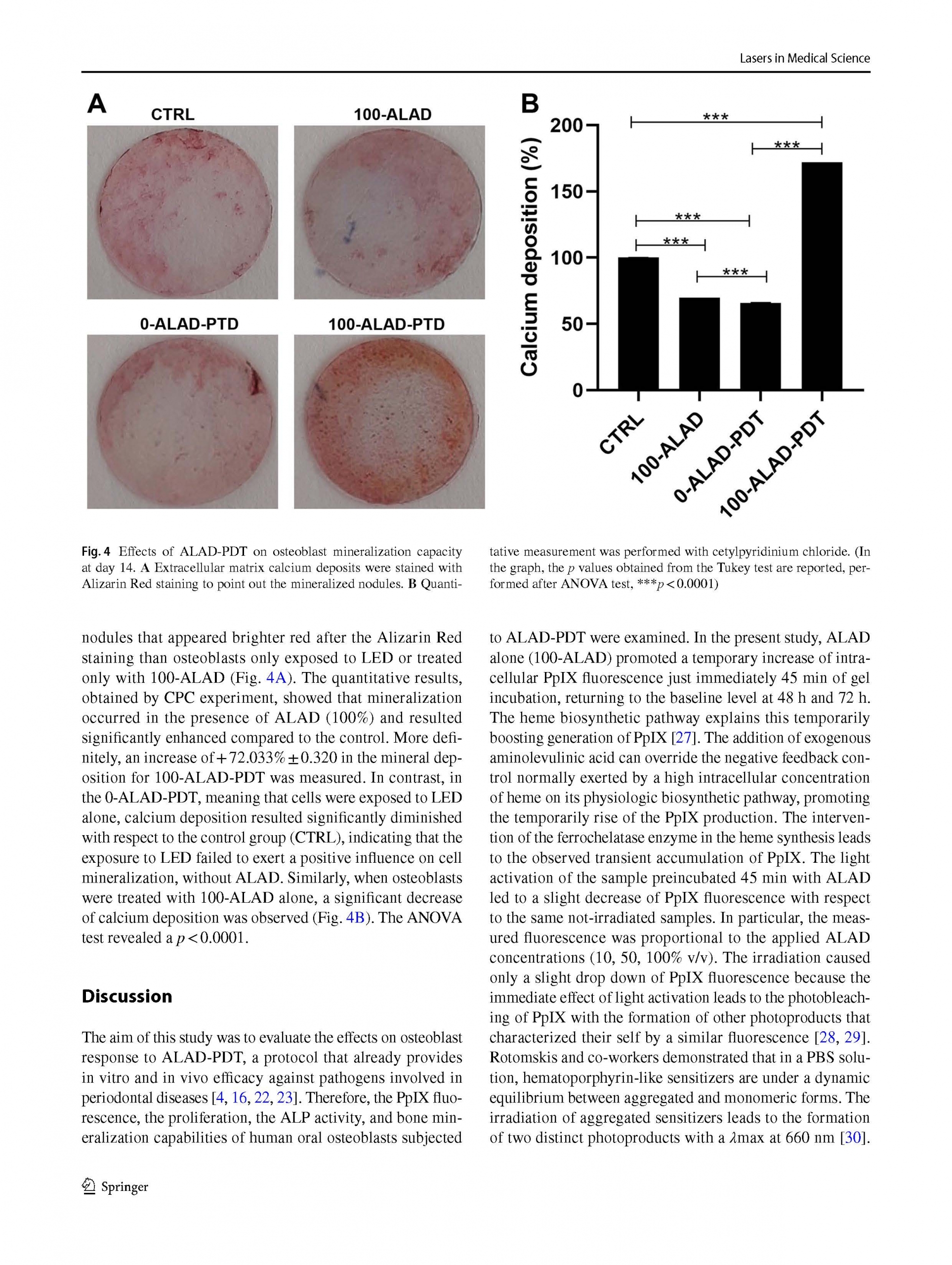
/in Pubblicazioni recenti /da q82rrfo3The osteoblastic cells incubated for 45 min with ALAD gel as commercialized and exposed for 7 min to the red light of 630 nm LED showed a statistical increase of cell growth, and a stimulatory effect on ALP activity and mineralization.




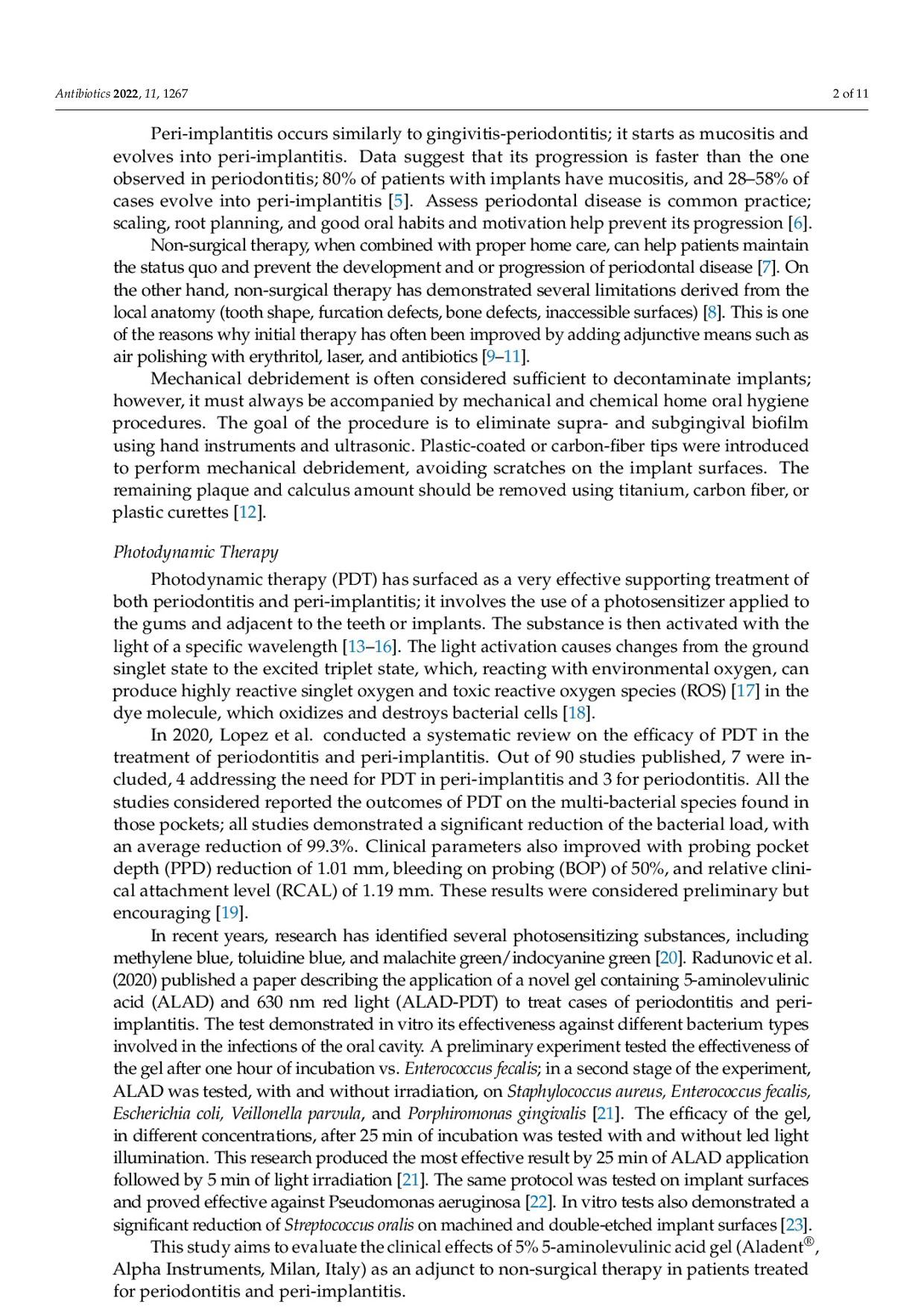
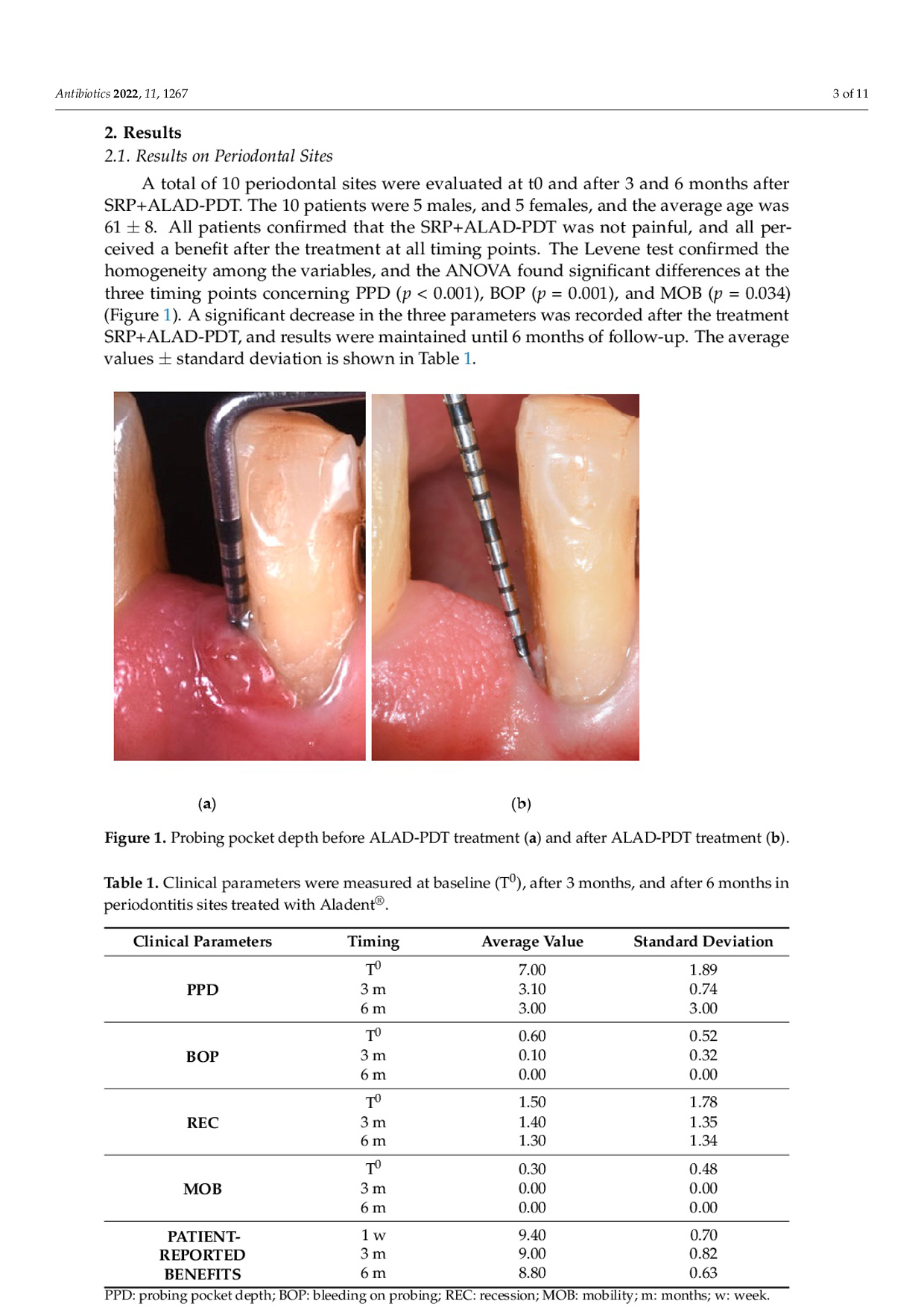
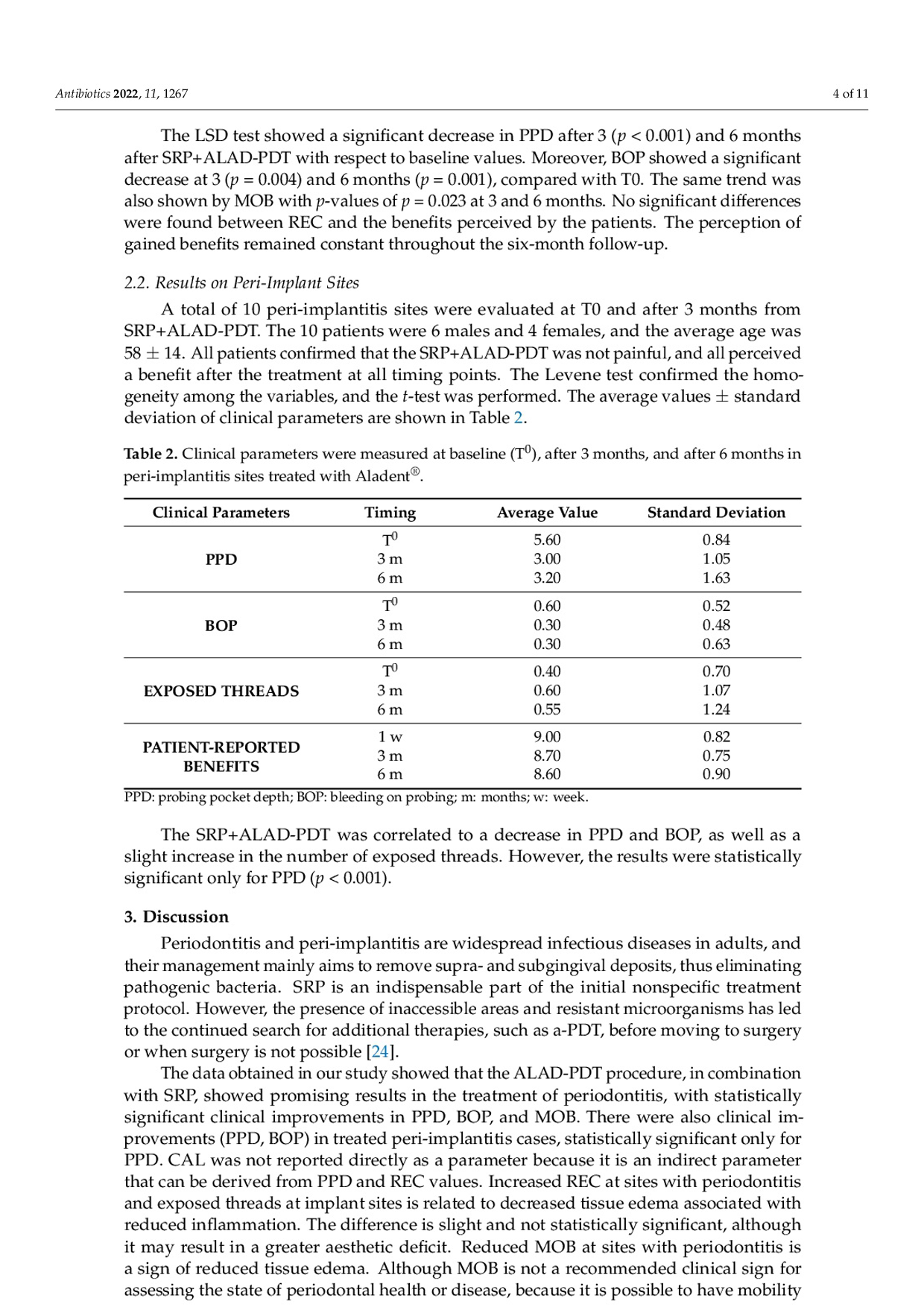
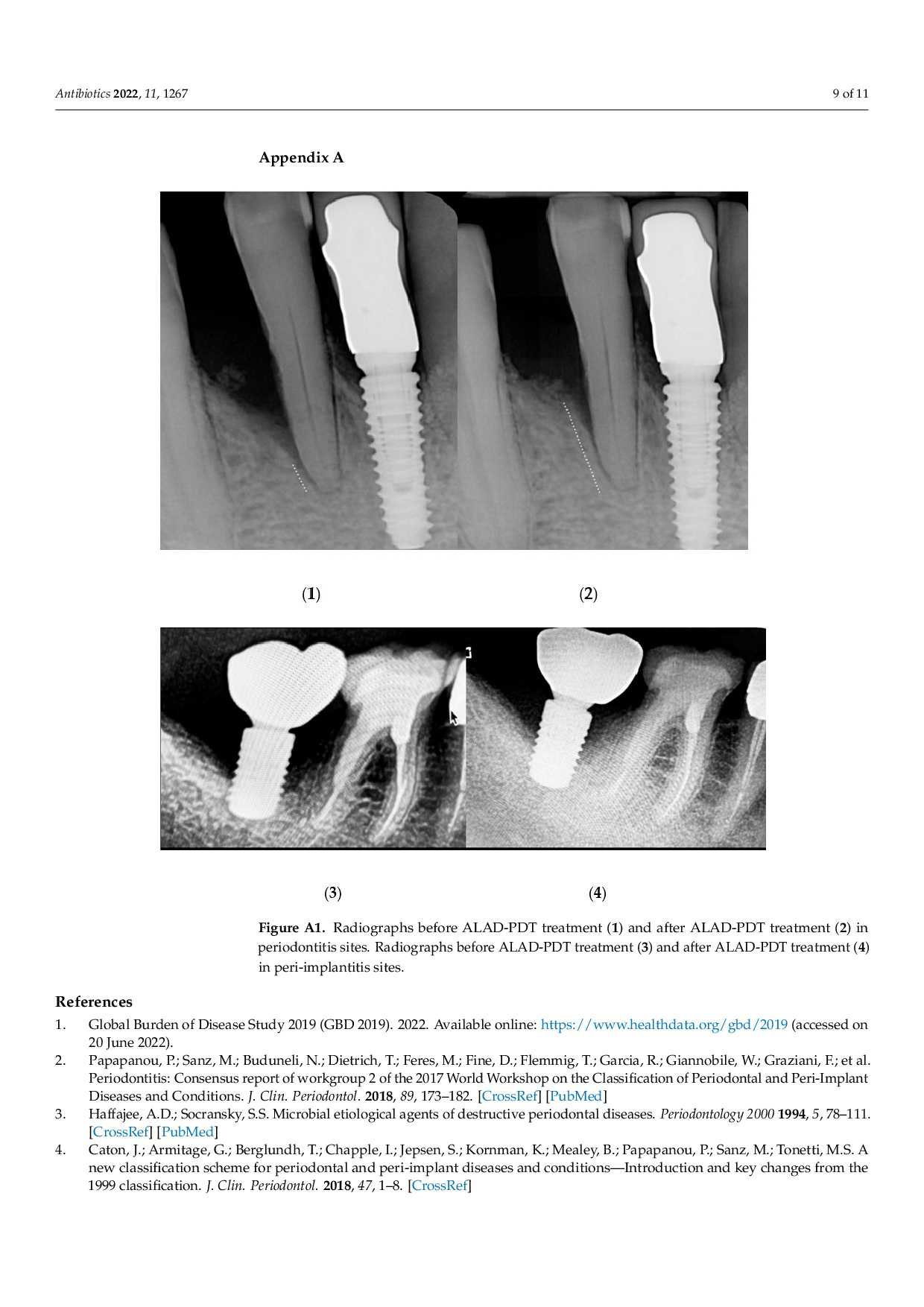
Photodynamic Therapy by Mean of 5 Aminolevulinic Acid for the Management of Periodontitis and Peri-Implantitis: a Retrospective Analysis of 20 Patients.
/in Pubblicazioni recenti /da q82rrfo3Photodynamic Therapy by Mean of 5 Aminolevulinic Acid for the Management of Periodontitis and Peri-Implantitis: a Retrospective Analysis of 20 Patients.
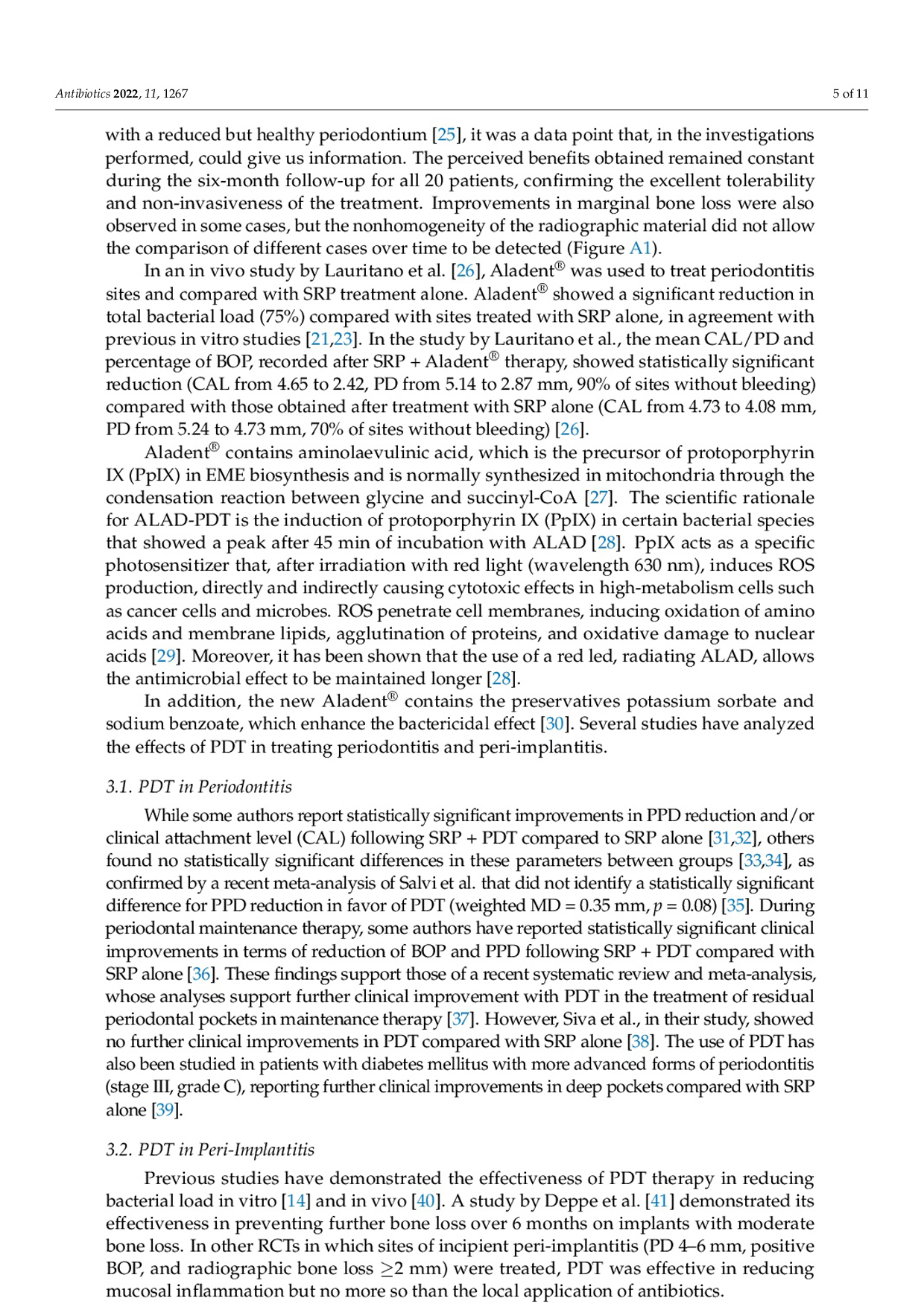
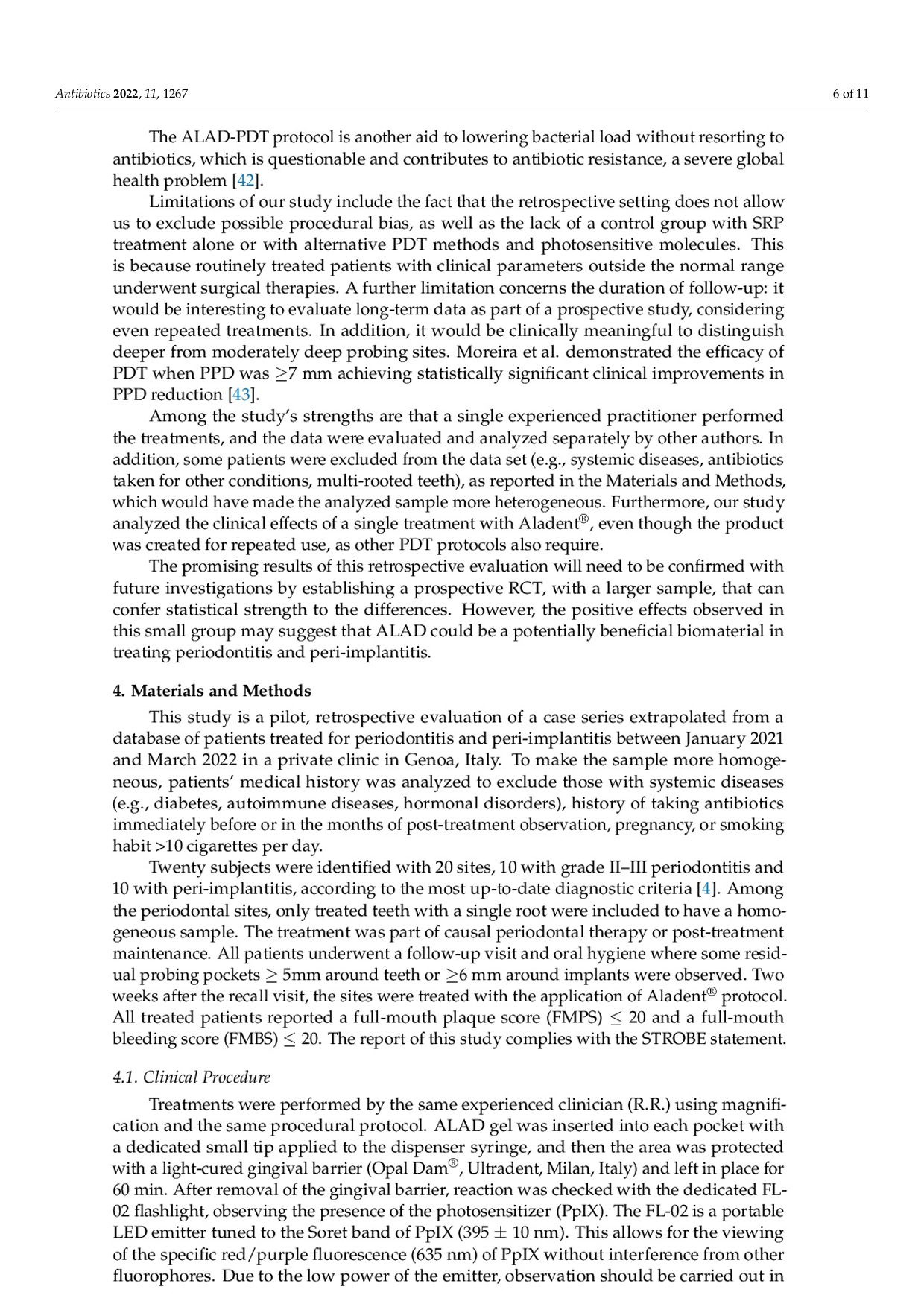
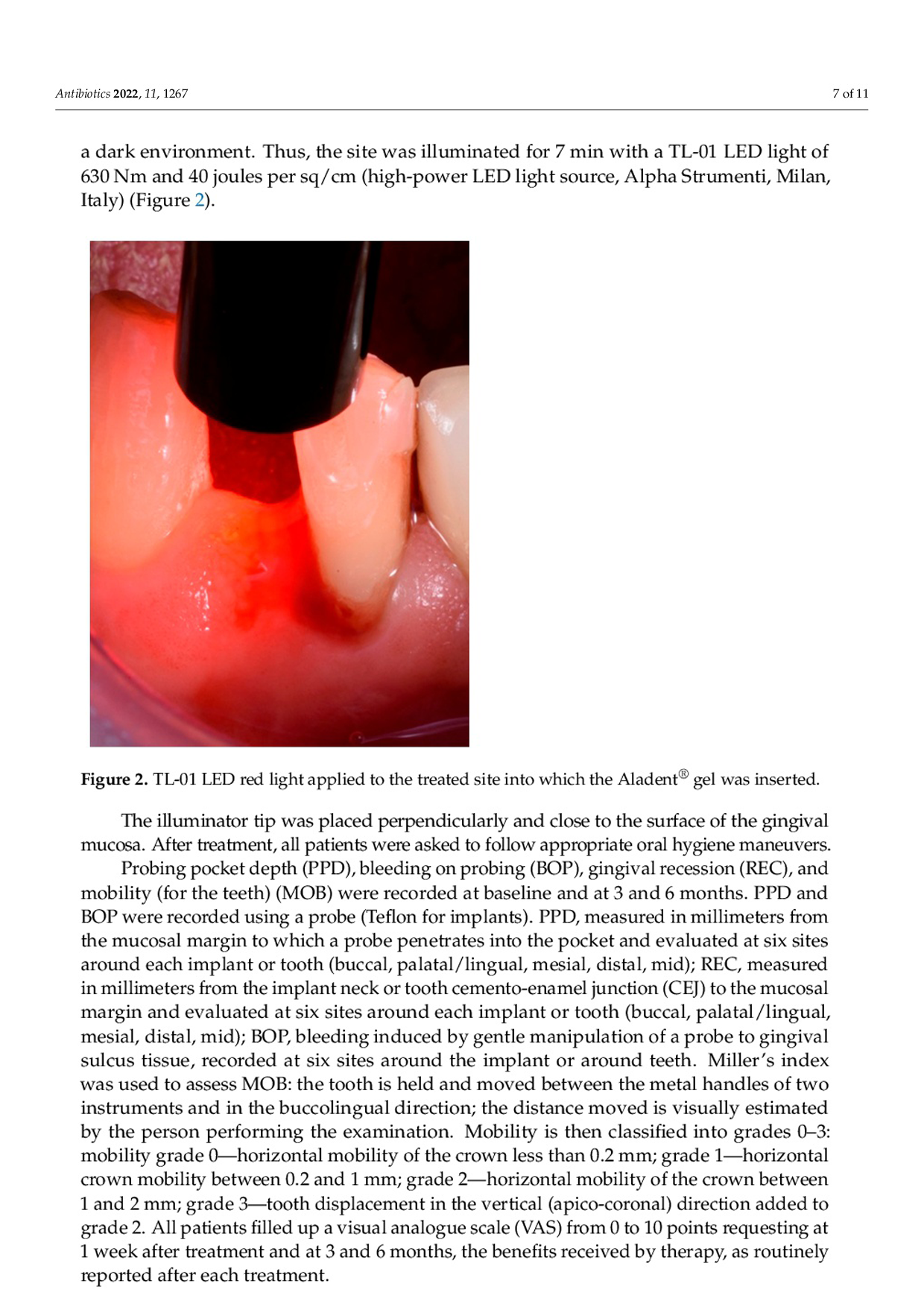
The articole showed that in periodontal patients, all sites evaluated had a beneficial effect on PPD, BOP, and MOB with statistically significant differences between baseline and at 3 and 6 months after. For the periimplantitis sites, all patients confirmed that the SRP+ALAD-PDT was not painful, and all perceived a benefit after the treatment at all timing points.

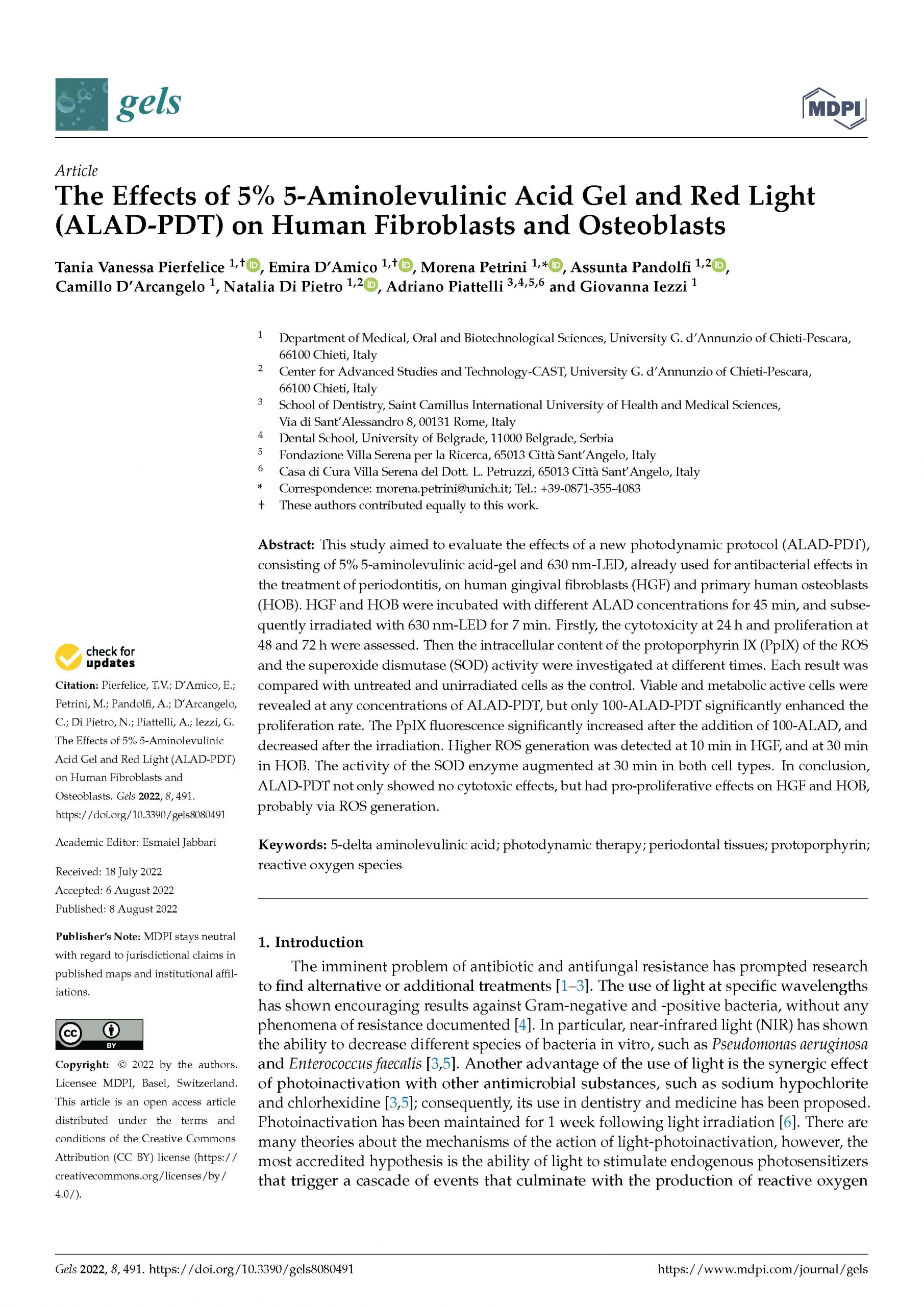
The Effects of 5% 5-Aminolevulinic Acid Gel and Red Light (ALAD-PDT) on Human Fibroblasts and Osteoblasts.
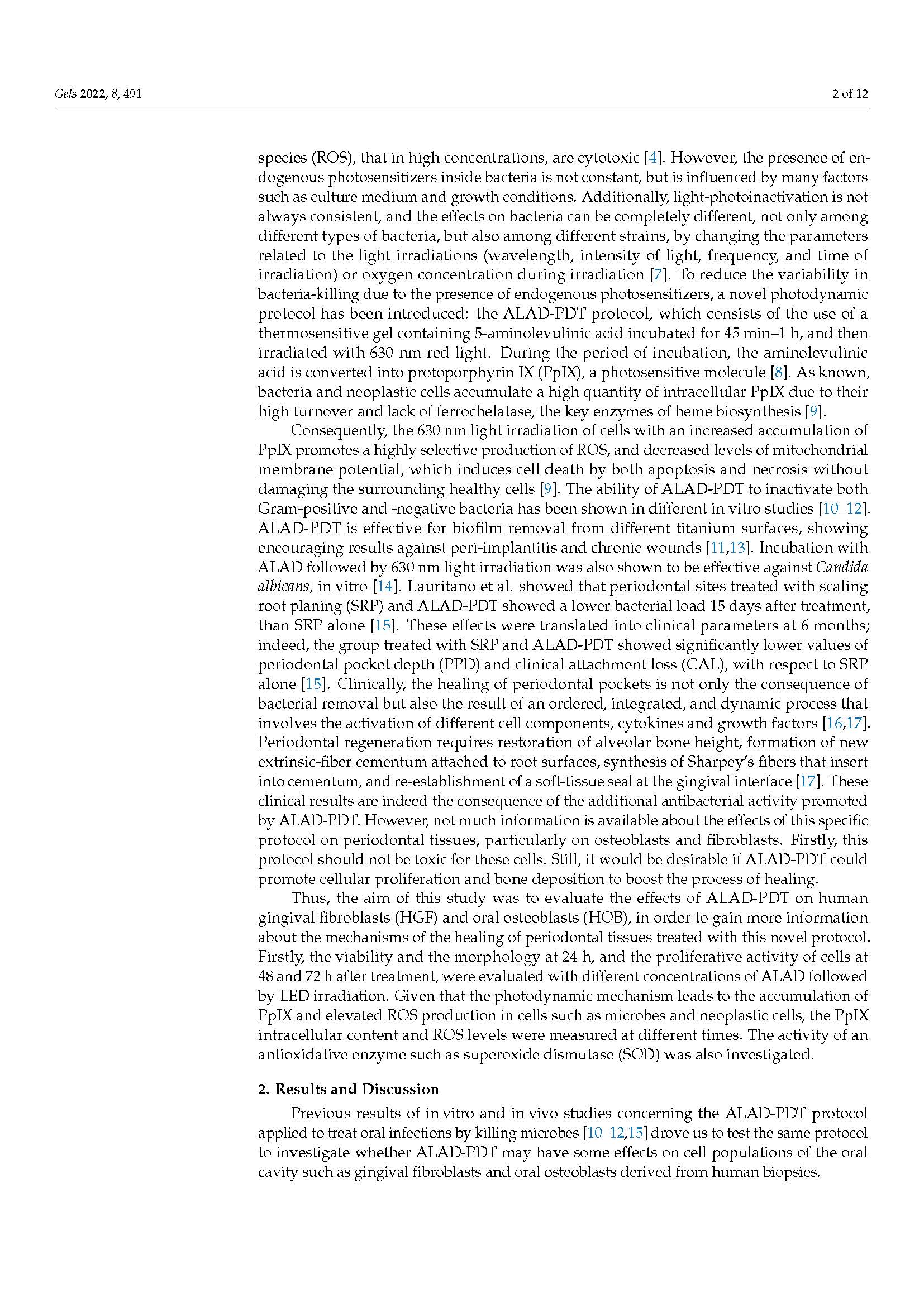
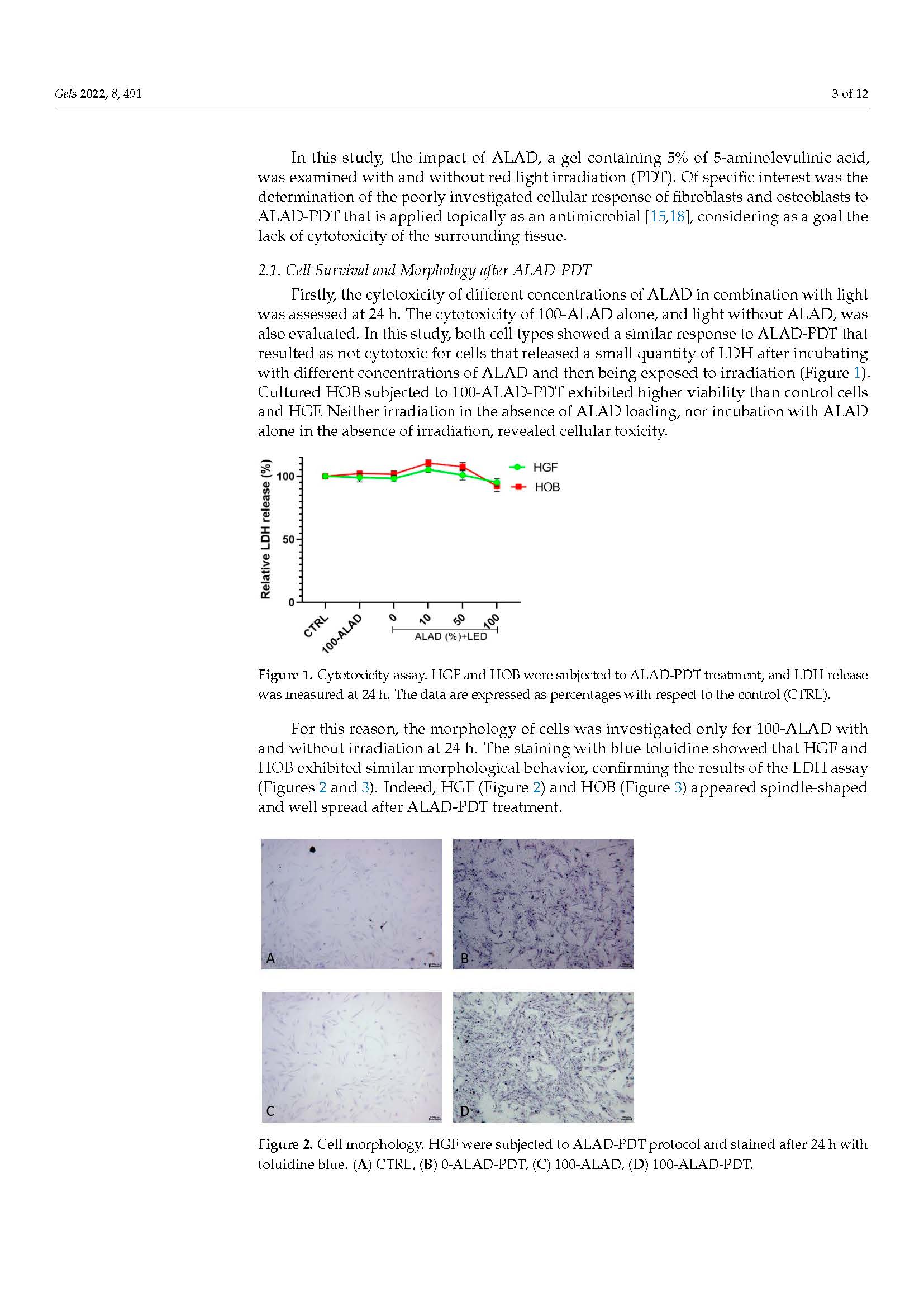
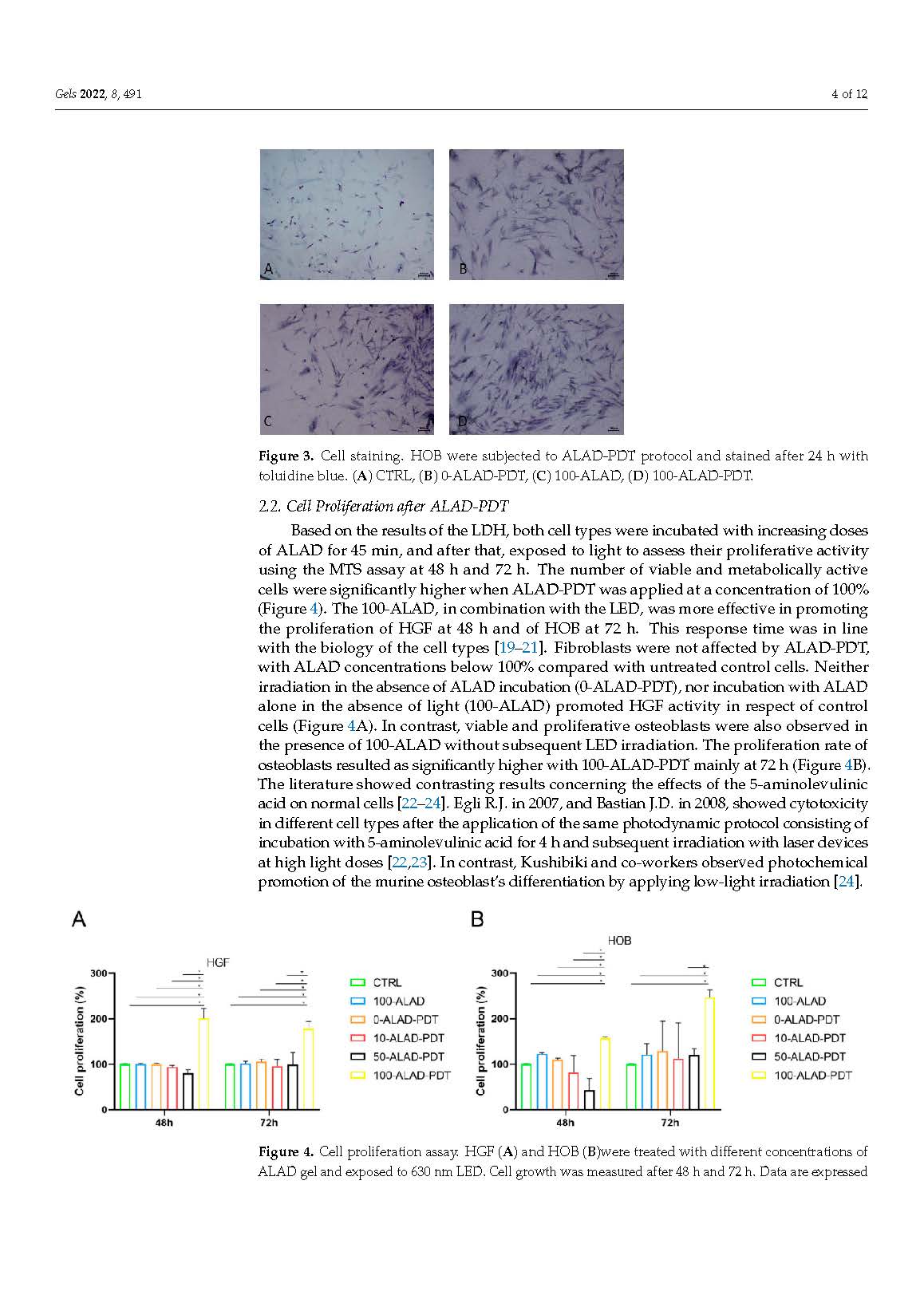
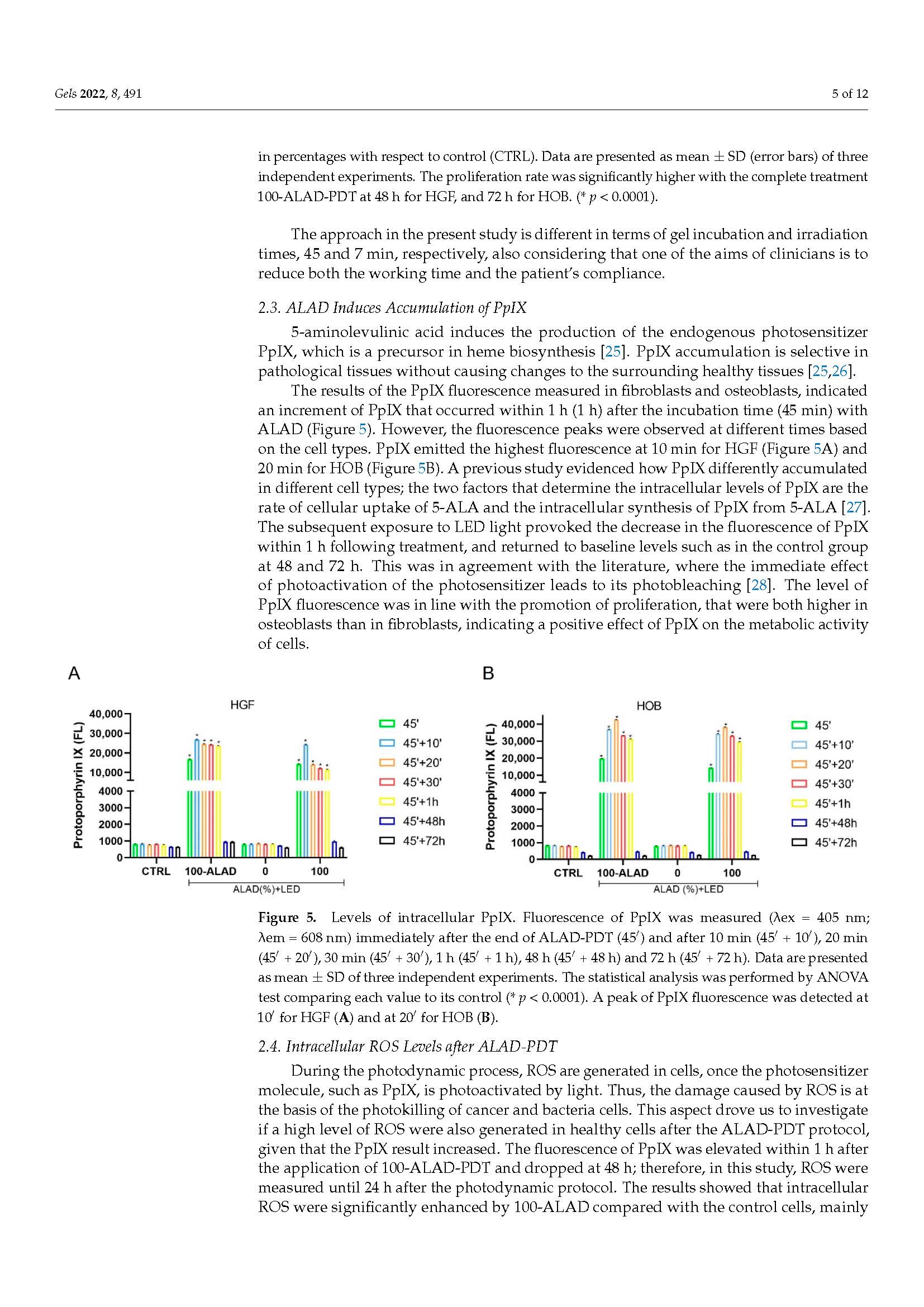
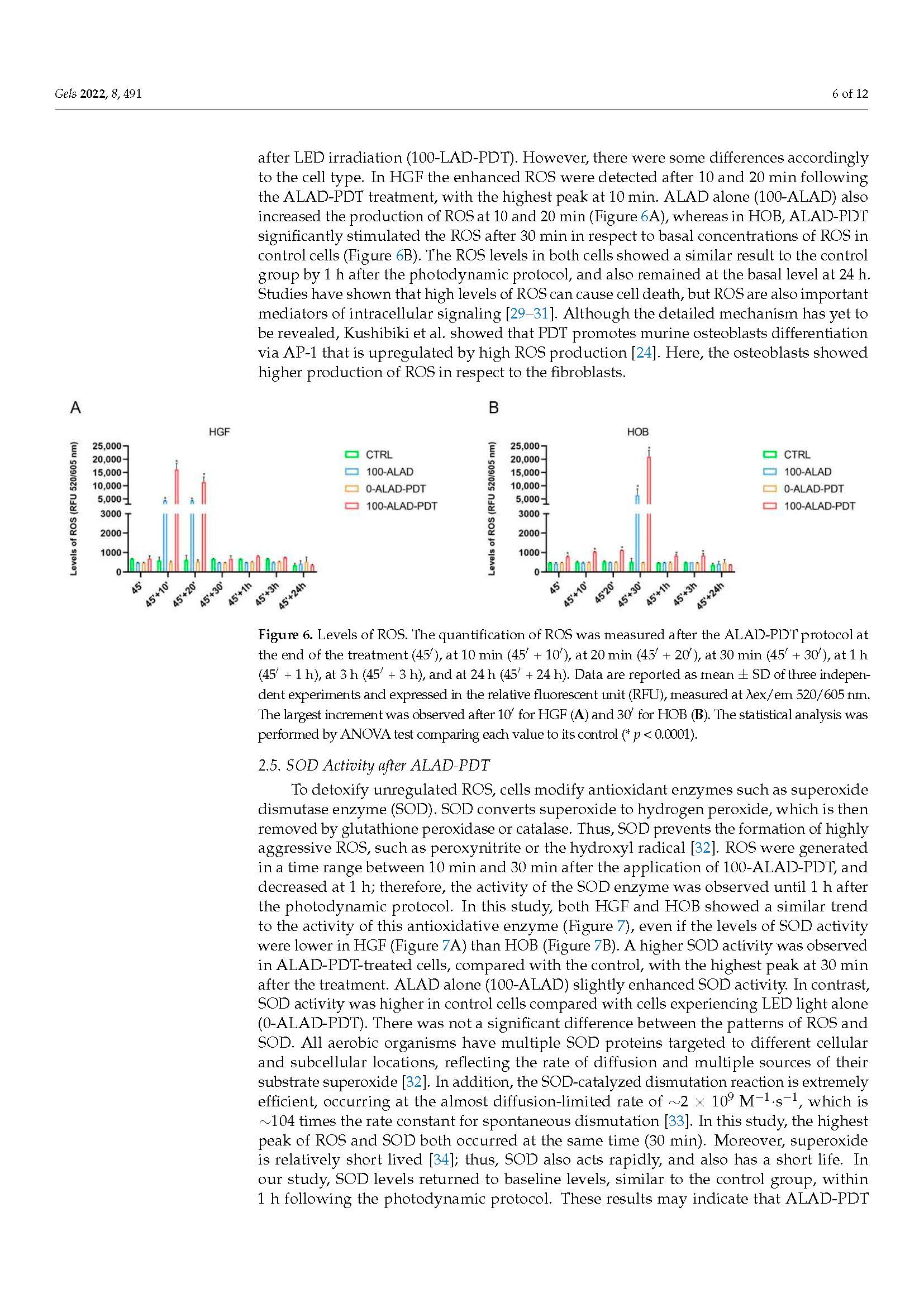
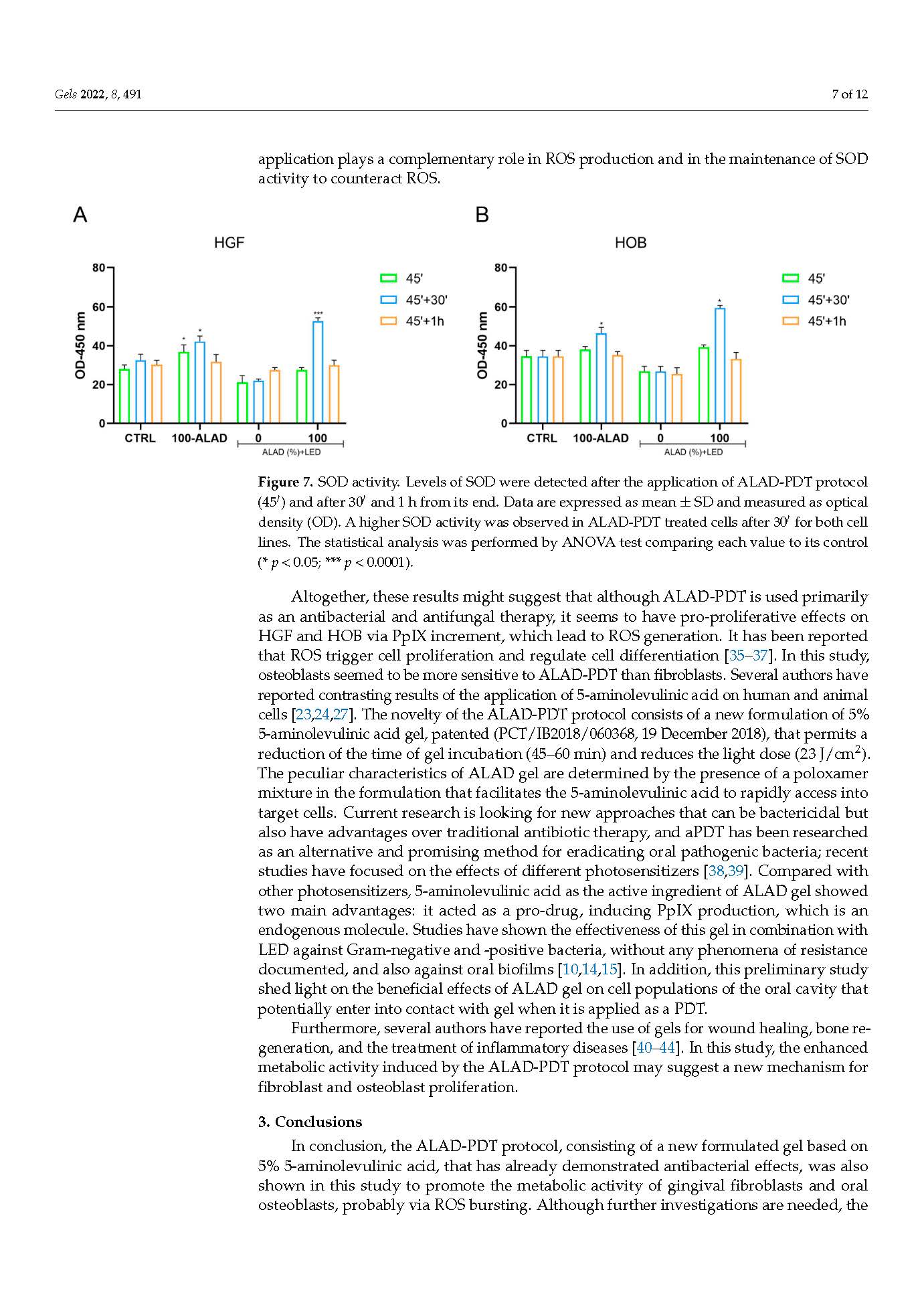
/in Pubblicazioni recenti /da q82rrfo3ALA-PDT protocol, consisting of a new formulated gel based on 5% 5-aminolevulinic acid, that has already demostrated antibacterial effects, was also shown in this study to promote the metabolic activity of gingival fibroblasts and oral osteoblast.
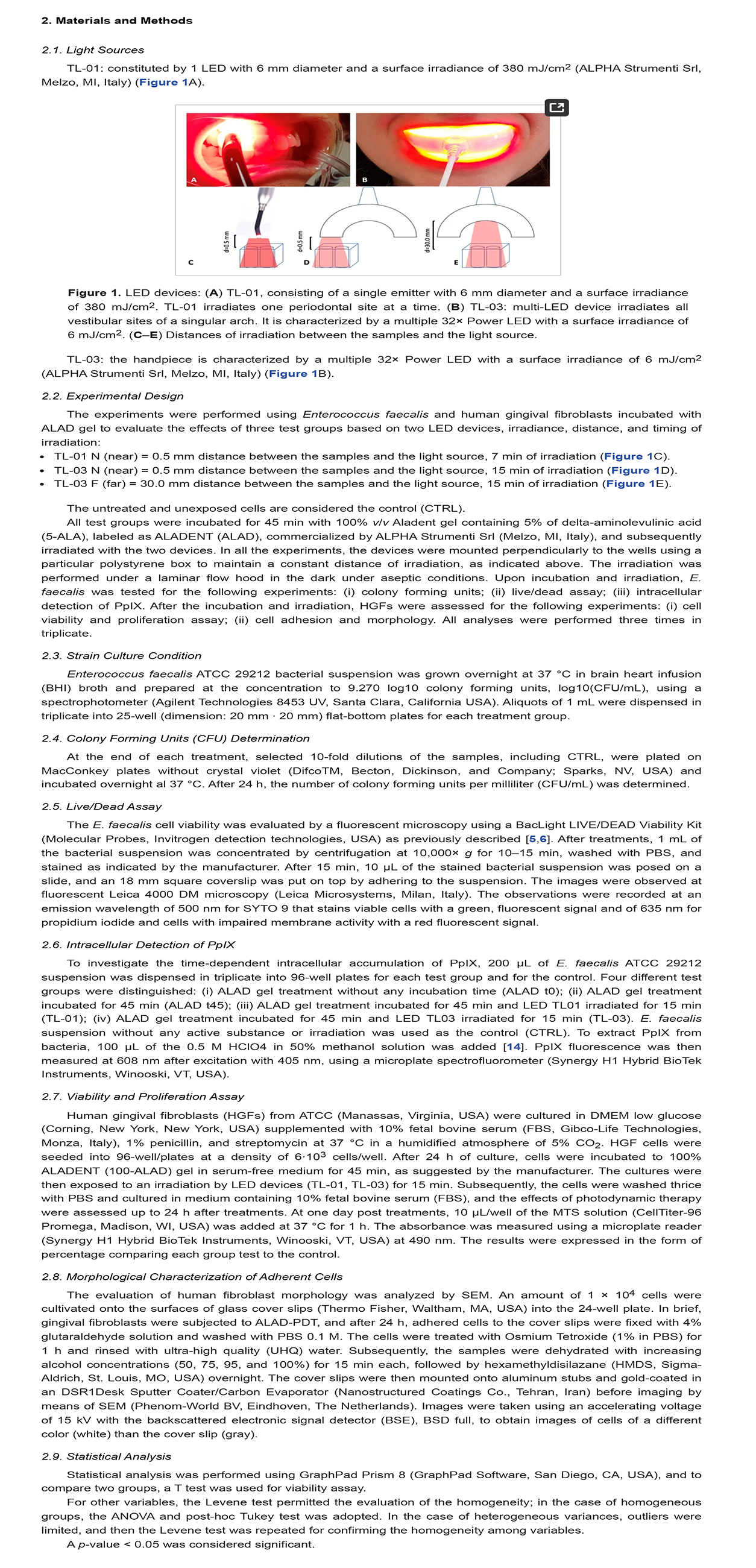
Comparison between Single and Multi-LED Emitters for Photodynamic Therapy: An In Vitro Study on Enterococcus faecalis and Human Gingival Fibroblasts.
/in Pubblicazioni recenti /da q82rrfo3Alphastrumenti Srl
Via Volontari del Sangue 4
20066 Melzo – MI
P.iva 06754120159
Email: info@aladent.it
Tel: +39.0295738540
Fax: +39.029551815